Image by cobalt123 via Flickr
Okay, here's the skinny on my recent health problems and hospital stay...
Two Saturdays ago I woke up feeling a bit out of sorts, which I attributed to my new Zanaflex prescription, which I'd only taken for two nights. My neuro had prescribed the medication for me because of incredibly annoying muscle spasms in my right leg, which were keeping me (and Karen) from getting to sleep at night. Definitely one of my most annoying MS symptoms, my leg often spasms so badly that the entire bed shakes, like a Japanese villager suddenly come face to face with Godzilla.
By mid afternoon that Saturday, I was feeling so unwell that I called my neuro's office, and spoke to the doctor on call, who I know quite well, and who is a terrific physician and person.
The doctor told me to quit taking Zanaflex, and increase my dosage of Klonopin. Fine, I thought, that's that. I tried to get on with my day .
Early that evening, at around 6 PM, I really started to feel like crap. I started losing strength in my left side (and I already have no strength in my right side), and began feeling achy and just not well. With much difficulty, I climbed into bed, and lay there under the covers, shivering. Karen had conked out on the living room couch, and I didn't want to bother her.
I fell asleep for a little while, but when I woke up, I was practically paralyzed. Yikes! I could barely move my left side at all, and found it impossible to try to get out of bed. Karen came in and took my temperature, which registered 99.5. For a person with a normal body temperature, 99.5° is barely a fever, but, like many MS patients, my normal body temperature is very low, usually around 97°. So, that 99.5° was more like 101.5° for a person whose baseline is the normal 98.6°.
The fever completely messed with my broken nervous system (that damned heat sensitivity thing), and left me with a useless body. Very disturbing, to say the least. I've learned in the years since my diagnosis that the symptoms brought on by fever are a harbinger of things to come in my disease course. This episode showed quite clearly what the future holds for me unless some intervention can put a stop to my disease progression. Not a comforting picture, in fact, quite distressing..
Karen called my neuro on his cell phone, and he told us to immediately go to the hospital emergency room. We explained that since I couldn't move, that would be kind of difficult. He insisted that we call for an ambulance. What a wonderful Saturday night. The ambulance arrived very quickly, and two quite strong female EMTs physically lifted me out of bed and onto the gurney, for the trip down the elevator, through the lobby of my building, and into the waiting ambulance. My first ever ambulance ride. How joyous.
We're suffering through one of the hottest July's on record here in New York, and the combination of my fever and the heat and humidity really knocked me out. I felt almost delirious, and Karen said I was speaking very slowly and slurring my words.
Once at the hospital, they did a bunch of blood tests, started me on a saline drip, and fed me some Tylenol. My fever reached all the way to 101.5° on their thermometers, meaning the equivalent for a non-MSer would be a fever of about 103.5°. After a long night in the emergency room, I was finally admitted to the hospital, and was given a room at about 6 AM.
Because I could barely move, I had to have a Foley catheter inserted, not a pleasant experience. For those of you who are blissfully ignorant of Foley catheters, they are a device that is snaked up your urethra and into your bladder, thereby facilitating "voiding". Oh boy, another thing I can cross off my bucket list! Note to my male readers: definitely avoid having things stuck up your wiener. Not that I should have to tell you that, but in case the thought ever crosses your mind, let it go. I'm sure the process is no more pleasant for females, but the nurse who did the deed told me that female anatomy presents less real estate to cross for the catheter to make it into the bladder. The device was a necessity, though, since I couldn't get out of bed to get to the bathroom, and, in all honesty, not having to worry about how I was going to pee was a great relief.
My hospital roommate was a 62-year-old homeless man who had a 22 inch open wound on his right calf. He was surly and belligerent to the doctors and nurses, and wouldn't answer me when I tried to make an introduction through the curtain that divided the room. In the meantime, the hospital staff was reticent to start me on any treatments, because my neuro is such a big name that they did want to do anything without his okay. I thought that was absolute bullshit, since I was obviously suffering from some kind of infection, and my neuro is not an infectious diseases expert. I kept asking for them to start me on some general antibiotic, but they insisted on waiting for blood test results and cultures. So basically it was Tylenol and saline, and I was miserable.
Sleep was almost impossible, as the Foley catheter necessitated my staying on my back, and I simply can't sleep on my back. Furthermore, my homeless man roommate talked to himself incessantly, not quite the bedtime lullaby I needed.
Karen was her usual wonderful self, providing company, comfort, and relief. We live only 10 blocks from the hospital, so Karen was able to visit as much as possible.
Since they were often loud and confrontational, I couldn't help but listen to my roommate's interactions with his doctors, and also with himself (not quite as loud and confrontational), and soon realized that although he was guarded and quarrelsome, he was also very intelligent. I picked up bits and pieces of his story as he chatted away to himself, and slowly pieced together that at one point in his life things had been relatively normal; he'd been married and had held a job as a cook, but somewhere along the way things went off the rails. He was clearly very sharp, and his chatter touched on a wide range of subjects, from history to philosophy to religion. Best I could tell, his wife left him, and he never recovered from the heartbreak.
I suppose most of us have experienced a heartbreak that we thought we'd never survive, one that crushed your spirit seemingly beyond recovery . Unlike the majority of us, though, for my roommate this nightmare became a reality. There was clearly some mental illness at play here, but whether that illness instigated or was the result of his wife's departure I could not tell. Late Sunday night, he tried to sing himself to sleep, and started quietly singing that old 70s soul tune "Have You Seen Her" (click here).
I see her face everywhere I go, in the streets and even in the picture show, have you seen her, tell me have you seen her? Oh I hear her voice as the cold winds blow, in the sweet music on my radio, have you seen her, tell me have you seen her?…
Maybe it was my fever and near delirium, but I found the whole thing very touching.
As it happens, I'm a huge fan of 70s soul music, and I have "Have You Seen Her" on the MP3 player that is integrated into my cell phone. During breakfast the next morning, I played the song through my phone's tinny speaker, and thus began a growing friendship between me and Greg, the homeless man. He was indeed very intelligent, had studied martial arts, was very knowledgeable about Zen and Taoism, was an expert on the use of herbs and plants as natural remedies, and was a big movie buff. He also was a little bit cuckoo, but who among us isn't? It dawned on me that he was belligerent simply because he'd been taken advantage of far too often, and he talked to himself probably because he usually had no one else to talk to. In one on one conversation, he was lucid and even dignified.
Anyway, even though all of my blood tests came back negative, late Monday I was seen by an infectious diseases doctor who immediately started me on antibiotics (azithromycin). My fever quickly came way down, and I started feeling much better. My neuro wanted me out of the hospital as soon as possible, since, in his words, "the only reason hospitals don't kill more people is because people are hard to kill".
As I was preparing to be discharged on Tuesday, the hospital staff informed my roommate Greg that he would have to leave the hospital within 24 hours, because there was no longer any medical reason to keep him there. They had tended to his wound, which he actually had taken very good care of himself, until he was caught in a rainstorm and the wound became wet and dirty, necessitating his hospitalization.
Unfortunately, once out of the hospital, Greg would have no place to go, and the hospital social worker was a complete bitch to him, offering only the option of going to a homeless shelter. He refused to go to one, because such shelters are filled with predators, and as a 62-year-old man with an open wound on his leg, he would be a quick target. He also refused to go to Bellevue, the New York City hospital for the indigent, because it is really no better than a prison. Karen and I let him use my cell phone for about an hour after I was officially discharged so that he could try to find some kind of better housing, which I believe he succeeded in doing. I'm not sure, though. I gave him my phone number, but he hasn't called, so I only hope that one of the leads he was following worked out. By the time I was discharged, this surly man who had just a few days before refused to even answer my attempts at conversation was referring to me as Marky Marc, and I felt a genuine bond between us.
One of my biggest surprises was finally getting a good look at Greg, as we had conducted virtually all of our conversations through the curtain that divided the hospital room. When I was leaving, I saw that Greg, though 62 years old, was built like the Incredible Hulk. Not bad for a man toughing it out on the streets of New York City.
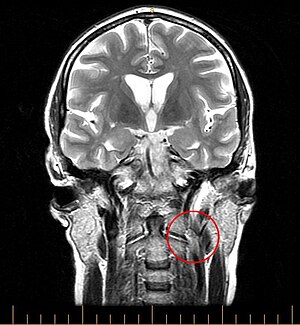
I'd say I'm now about 80% healthy, but the whole experience definitely was a call to action. As I said before, the fever served as a sneak preview of the direction my illness is headed, and it isn't good. I must vigorously pursue the CCSVI angle, as I know that I do have a severely blocked jugular, and at the very least, that can't be doing me any good. I have little to lose, and I clearly must take the most aggressive posture possible.
All in all, this was certainly one of life's more interesting episodes. There I was, feeling like crap, scared shitless, forced out of the "now" to stare at the possibility of a miserable future. And there was Greg, the voice across the curtain, a bundle of lessons to be learned, not the least of which was perseverance and dignity in the face of constant struggle. Maybe there really is no such thing as coincidence...
To those readers who have sent e-mails over the last couple of weeks, I will try to answer every one, but please be patient. I'm trying not to overdo things, as I really don't want to risk another fever...