When I started this blog, I decided I didn't want it to be a blow-by-blow account of my journey through the medical world, a symptom diary, or a journal of the treatment regimens I've attempted. Instead, I've tried to emphasize the emotional and psychological challenges shared by patients forced to confront a chronic debilitating disease, and also make it a place to report on and attempt to interpret much of the MS research I find myself obsessively compelled to seek out. Occasionally, though, I've deviated from that path when events of enough medical interest crop up as I deal with my disease, and I recently experienced just such a development.
Long time (and even some short time) readers of this blog probably know that I'm something of a mystery patient, as my diagnosis has been up in the air for quite some time. I was first diagnosed with "atypical Primary Progressive Multiple Sclerosis" back in 2004, about a year after my first symptom – a slight limp in my right leg – showed itself. My disease was considered atypical because my MRIs revealed only one significant lesion (a big juicy one at the base of my brainstem, an especially bad place to have one), lumbar punctures showed no O-bands or other CSF abnormalities, my medical history hinted at some kind of systemic autoimmune disorder, and I generally didn't conform to the any of the diagnostic criteria (click here) established for the different forms of MS.
I ditched my first MS neurologist after a year because, despite his being a fine physician, he had the personality of a herring. My second MS neurologist immediately suspected that I might not have multiple sclerosis and had me tested for a host of different diseases that might account for my symptoms, including sarcoidosis, lupus, Hughes syndrome, Lyme disease, and others. When none of these tests came back positive, I was slapped with that "atypical PPMS" label again, and for several years that's where things stood.
Never comfortable with my diagnosis, I pursued other opinions, my efforts including visits to the Johns Hopkins MS Center on two separate occasions. The doctors at Johns Hopkins finally told me that it was indeed quite likely that I did not suffer from MS, primarily because, along with all of the other strange elements of my presentation, my lesion had not changed at all in size or shape since it first been imaged several years earlier (it remains unchanged to this day), nor had it been joined by any others. These fine physicians couldn't quite put a finger on precisely what might be ailing me, though. They suggested I be tested for Sjogren's disease and also that I consult with a mitochondrial disease specialist. I did both and came up with nada.
At about that time I was accepted into a research study being conducted by the National Institutes of Health, the US government's medical research arm, whose primary facility is located in Bethesda, Maryland. The study was designed specifically to identify clinically definite MS patients. During my four visits to the NIH, I was subjected to almost every conceivable diagnostic test, and had enough blood drawn to feed a vampire family of four for at least a month. After all the testing was complete, the NIH agreed with the doctors at Johns Hopkins, saying that although I definitely couldn't be classified as having clinically definite MS, they couldn't come up with a viable alternate diagnosis. So, for the last 18 months or so, I've been stuck in a kind of never never land as far as my diagnosis goes. My local neurologist, no slouch in his own right, has by and large stuck with the "atypical PPMS" diagnosis, since MS is a diagnosis of exclusion, and we've excluded every other possibility we could think of.
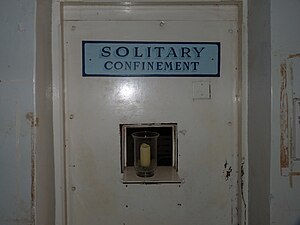
Recently, the NIH has decided that I could very likely be suffering from "Solitary Sclerosis", a condition that was recently described in a paper published by researchers at the Mayo Clinic (click here). The paper details seven patients who presented with progressive disability and only one visible lesion on their MRI images, all at the cervicomedullary junction, precisely where my lesion is located. Although my lesion (I've named it Adolph) has a number of very atypical features, and much of the other strangeness about my case hasn't been resolved, the NIH doctors feel that this newly described derivation of MS is the closest fit for my condition. I'm actually a little bit confused by this, because the folks at the NIH originally presented quite a long list of reasons why they didn't think I had MS, many of which now seem to have been minimized in order to make the Solitary Sclerosis diagnosis fit, but I will concede that this newly identified MS offshoot does cover some of the more glaring anomalies surrounding my condition.
It may seem strange, but I've actually grown kind of comfortable not having a definite diagnosis, since having no diagnosis leaves open the possibility of any conceivable outcome, including total recovery. Solitary Sclerosis doesn't seem to be an especially cheerful diagnosis, as of the seven patients the researchers looked at, one is dead, two are quadriplegics and completely bedridden, and the other four are quite disabled and progressing rather rapidly. None of the SS patients responded positively to any of the standard MS disease modifying drugs, which is typical for patients suffering from the progressive forms of Multiple Sclerosis.
I too haven't had much luck with the many MS therapies I've tried, although I did once get tremendous benefit from a large prolonged dose of IV steroids (which unfortunately later caused me to develop avascular necrosis (click here), an excruciating condition which I wouldn't wish on anybody), and I initially did surprisingly well on IVIG, which would be highly unusual for a patient suffering from a progressive form of MS. Overall, I'm still quite dubious of the SS designation, since I continue to have all kinds of weirdness associated with my disease, and as I've cut my swath through the medical community I've certainly left enough doctors scratching their heads in my wake.
I'm currently pursuing a few different diagnostic possibilities, which I'll report on if any turn out to be worthwhile enough to write about. But, for the time being, I have at least one foot (the gimpy one) planted in the MS camp, as a possible (probable?) Solitary Sclerosis patient. On the bright side, I'm quite likely the first ever Jewish member of the SS, quite fitting for a patient who long ago named his lesion Adolph.
Yes, nothing like some horribly distasteful humor to finish up an otherwise serious blog post…

OMG. Solitary Sclerosis. You mean this many-headed hydra has yet another offshoot?
ReplyDeleteI have a feeling it has many offshoots, and that eventually we will see that our current understanding of MS is tremendously limited. We are starting to see hints (and sometimes much more than hints) that much of what's taken for granted about MS may be entirely wrong, and modern medicine may need to rethink the disease and the strategies used to cope with it.
DeleteFive years ago when I was diagnosed I remember my neurologist saying that she wouldn't be surprised if my diagnosis changed. I was a bit surprised. I asked if that meant I would get better (always the optimist!) She said many doctors believed what was being diagnosed as MS now would later be segmented in to a dozen or more different diagnosis. She called it the "business casual" diagnosis...lots of things fit but it was difficult define.
ReplyDeleteOne of the main problems is that MS is a diagnosis by exclusion, as there are no tests that specifically indicate a patient has multiple sclerosis. Instead, doctors try to rule out any other possible causes for a patient's symptoms, and once that's done, they assume a diagnosis of MS.
DeleteIf a patient has a classic case, with a brain full of lesions and spinal fluid that shows multiple O-bands, then the diagnosis seems to be fairly reliable. For those of us who fall outside of that narrow definition, though, diagnosis is a much trickier business.
It's estimated that the misdiagnosis rate of MS is between 5%-15%. Way too high…
I just read this article http://medicalxpress.com/news/2012-05-misdiagnosis-ms-health-millions-year.html about MS being commonly misdiagnosed. I was bummed the article did not go into what most of the patients actually ended up suffering from and how they figured it out. The article's main concern was how much treating with expensive therapies was costing the taxpayers. And a little bit about how the injectees were suffering side effects needlessly. I loved the coincidence of 'Adolph' and SS. Sometimes humor is the only thing left in a situation. Thanks for keeping us posted.
ReplyDeleteI read that same article, and I would assume that the patients' actual diagnoses were a wide range of diseases. There are over 100 diseases that can look like MS, from Lyme disease to other autoimmune diseases to vascular problems (and I'm not talking about CCSVI).
DeleteWithout humor life simply wouldn't be worth living. We are all just players in a big theater of the absurd…
Without a doubt you have had the most interesting journey of anyone I've heard of who has/might have MS, (and I know how thrilled you are to be so "interesting"). Honestly, what you have/don't have is just as amazing as you, yourself. I'm always jumping to read your next post.
ReplyDeleteThanks for all the information, cheer, straight talk, knock-my-socks-off art, helpful personal insights that all too often apply to me as well, and for being so willing to serve the community.
Thank you, flattery will get you everywhere.
DeleteIt has been an interesting journey, and has reawakened my inner scientist, but I would have much rather the alarm clock has been something a bit less threatening. Dealing with my disease has definitely changed me, in both positive and negative ways, but really, I'm ready for it to stop. Really. Really really.
It's that kind of attitude that makes me like you.
ReplyDeletekicker
And it's that kind of attitude that makes me like you. I like people who like me. Except for the people who like me that I don't like, they can be really annoying. It's worse when somebody you like doesn't like you, though. Mutual dislike his okay, but it's funny how sometimes people with whom you share a mutual dislike can turn into good friends, given the proper circumstances.
DeleteLet's face it, along with the world being a huge theater of the absurd, it's also a big seventh-grade class, filled with insecure folks trying their hardest to keep their shit together. Some just play the game better than others…
Great post! Seems we all share a solitary side to our sclerosis. Sad but true you aren't alone. I do feel however you should rename Adolph to asshole.
ReplyDeleteHow about Adolph Asshole? A single lesion that's doing that much damage certainly deserves two names. Maybe even a middle initial. Adolph J Asshole,Esquire.
DeleteI am not sure how helpful the diagnosis is. It describes the condition of solitary sclerosis (and that the solitary sclerosis was located in the same place in these different patients seems to suggest that all 7 patients have the same disease) but there is no treatment, no explanation of the cause, and the prognosis is less than rosy. I am waiting to hear more about the vascular abnormality at the same level as the sclerosis, and do these other patients have the same vascular abnormality, and can it be treated. It might be simplistic to always look for a vascular explanation but it was what worked for me, and the only thing that has worked for me. If some of the other patients with solitary sclerosis have the same vascular abnormality, that would be suggestive of what the problem is, and from that, the solution.
ReplyDeleteIt would be great if the answer was that simple, but the doctors doing CCSVI treatment all report that they are finding little correlation between areas of vascular abnormality and specific forms of the disease. While I'm not discounting that there could be a vascular component to SS, I really doubt that the same vascular malformation would be seen in all patients.
DeleteI'm thrilled that CCSVI worked for you, but it doesn't work for a significant segment of the MS population, and most of the reports indicate that it's less effective on people with progressive illness.
It would be fantastic if as simplistic an answer as a shared vascular abnormality could be found that explained away not only assess but all forms of MS, unfortunately that's a dream not likely to be realized.
I tend to believe the current classifications of "M.S." are inadequate and outdated. They perhaps make things simpler for the medical/research/insurance/drug folks but although I can now easily put myself into the SPMS category, there were many years when that could not be done by my neurologists. I know I share certain things with many others, whatever you call it. There are lots of exceptions and given how little we know about M.S., its actually makes sense that there is a fair amount of imprecision.
ReplyDeleteWhat's really incredible is how much imprecision there actually is in many areas of medicine. The amount that is absolutely known about most neurological diseases is quite small, most remain largely mysterious. Doctors just don't like to say "I don't know", so instead slap a label on a condition just to give themselves and their patients something to hold onto.
DeleteAs you note, some of this is due to financial considerations, has the insurance companies will approve certain treatments for certain diseases, or forms of diseases, but not for others.
Hi. I have only read your blog today, but WOW what an eyeopener! I have recently been diagnosed with SS after 4years , I too have just one lesion on my brainstem. No one including my doctors and neurologist seem that bothered despite the fact my left arm and leg (walking) is getting worse!
ReplyDeleteGlad that you discovered my blog, but sorry that you're also a member of the SS. As you very well know, if you're going to only have one lesion, the base of the brainstem is a really bad spot to have it, unfortunately.
DeleteSeems that your doctors should be concerned that you are getting worse, but the fact that they really can't do much about it probably dampens their ability to seem bothered. I can understand their frustrations, but rather than various out of their offices, I do wish they'd try harder to fix us. Not that there aren't many hard-working, compassionate doctors out there, but I hear from way too many patients that their neurologists are assholes…
PS~ I featured your photography on my decorating blog. I hope that is ok? Your photos and writing are so very moving. Gosh, I probably should have asked first. I really would love to use a photo on my Chronic Healing blog, but I am too tired to write anymore. Sorry for the obsessive commenting.Thank you again.
DeleteOlivia
No problem, I'm honored to have you feature some of my photos in your decorating blog, as long as you mentioned where you found them… No worries about obsessive commenting, flattery will get you everywhere, and besides, interactivity is what makes a blog "alive"…
DeleteWow! Wow! Wow! I am so thankful to have read this post! My journey started six months ago. My MRI's are clean (so far). My LP shows no bands. Blood tests are pretty good. My nerve conduction study is the only thing that shows the widespread demylenation my body has been hit with. My neurologist has put me on the wait and see probable Multiple Sclerosis shelf. He offered to send me on to a University research center, but I need a break from doctors and tests. I have embraced the "probable MS label" and I am cruising the web comparing symptoms, alternative therapies etc... My feet have sustained the most damage. I can walk, but not for long periods or distances without my right foot completely seizing up. I am doing yoga twice/day, meditation, and whole foods. I am trying like hell to believe that the only thing stronger than fear is hope! So here is to hope that we don't nutt out in the unofficially diagnosed body whacking out category. Thank you for sharing. I am also trying to blog about keeping the warrior inside of me alive...my children are small so there is no other option, really. Hugs and light sent your way!
ReplyDeleteOlivia
Sorry to hear about your own unresolved diagnostic situation. It can all get so damned frustrating. Sounds like you are pursuing the right avenues, though, and not letting this thing get the better of you. Learn as much as you can, and be sure to be your own best advocate. Sending well wishes your way…
Delete~i am adding you to my sidebar, thank you or being brave, thank you for being a voice, i got a feeling there are more people stuck in solitary than we know....
ReplyDeleteMarc,
ReplyDeleteSorry to break this to you: you're not the only Jewish guy with SS (Jews always have problems with anything named "SS").
I'm 62, was diagnosed with transverse myelitis at age 50, and seemed to make a full recovery from the partial lesion at C2. Years later, I started to develop progressive symptoms despite the fact I don't have brain lesions and my primary lesion has not changed since the original diagnosis. Same course as your's, although i have yet to "graduate" to a wheelchair.
I wish I could say I've developed some great insight as a result of this experience. One just moves forward; there is no other way. I wish you well.
Fred Pritzker