It's now been about 16 months since the first Multiple Sclerosis patients outside of Italy underwent the venoplasty treatment known as The Liberation Procedure to address the then little heard of vascular condition termed "Chronic Cerebrospinal Venous Insufficiency", or CCSVI for short. Discovered earlier in the decade by the Italian vascular physician Dr. Paolo Zamboni, whose published papers reported success rates previously unheard of in the treatment of MS, knowledge of the condition and its potential relationship to MS was at that time scant, with few people in the MS community having ever heard of CCSVI. Those that were aware of the vascular hypothesis were confined, for the most part, to a small group of patients actively debating the relative merits and deficiencies of the hypothesis on one somewhat obscure MS Internet forum.
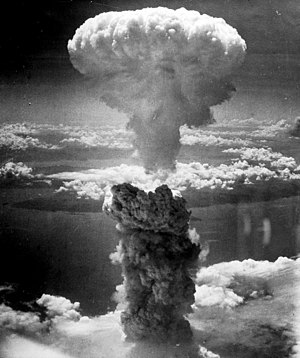
Well, what a difference 16 months make. The small trickle of patients undergoing treatment has now become, if not quite a flood, then at the very least an ever-increasing cascade, and word of CCSVI has spread like a kerosene fueled inferno throughout the MS population. Indeed, the very landscape of the Multiple Sclerosis world has shifted, as seismic waves of hope, promise, and controversy have swept over the horizon. In some cases, battle lines have been drawn, and in others, alliances formed. Fairly or not, in the eyes of many MS patients, mainstream neurology and the MS societies have become the enemy, mired in an outdated medical dogma and held in the sway of Big Pharma, and interventional radiologists following in Zamboni's footsteps have been hailed as conquering heroes.
Some of the first US doctors to start performing the Liberation Procedure were soon stopped by wary hospital administrators, but a handful of interventional radiologists in the United States are still openly doing the work, and a network of physicians operating "under the radar" has formed, their names being furtively passed from patient to patient via e-mail and social networking internet sites. Internationally, clinics offering the procedure are popping up from Costa Rica to Bulgaria, and the business of CCSVI medical tourism is booming. YouTube is bursting with videos of patients displaying their post-liberation gains, and web forums are abuzz with CCSVI chatter. Nonprofit CCSVI advocacy groups have formed, and patients, after years of being dictated to, are finally enjoying the self empowerment of having their say.
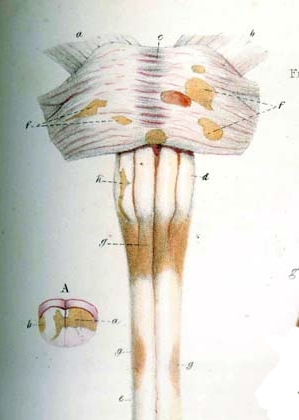
Put in its simplest terms, the CCSVI hypothesis states that blockages in the jugular and azygous veins, which drain the brain and spinal cord respectively, cause a long-term disruption in the flow of blood through the central nervous system, thus causing, over a period of many years, the damage to nervous system tissues that has come to be called Multiple Sclerosis. This relatively straightforward but radical notion flies in the face of accepted Multiple Sclerosis doctrine, which states that MS is an autoimmune disease caused by an immune system gone awry, and for reasons still unknown goes on a cannibalistic attack of a patient's own tissues. Though at first glance appearing to be at odds, in some ways the two theories actually complement each other, as CCSVI offers an explanation as to how and why immune system cells, which normally are stopped from infiltrating the central nervous system, can find their way through the blood brain barrier to wreak havoc on the nervous system beyond.
So, the CCSVI revolution rockets onward, an irreconcilable force destined to redefine, at a very basic level, medical science’s understanding of one of its greatest mysteries, the mechanism behind MS and maybe even some other autoimmune diseases, right?
Well, not so fast. Despite the boundless optimism expressed by many MS patients, there are still many very legitimate questions that need to be answered about the CCSVI hypothesis and the Liberation Procedure, questions impacting both near and long-term implications for the Multiple Sclerosis universe.
On a pathophysiological level, while CCSVI does seem to answer many of the perplexing questions surrounding MS, in some very important areas the hypothesis fails to reconcile with some firmly established facts about the disease. Among the most glaring examples of these are:
- The geographic distribution of the disease, which shows that the prevalence of MS increases indisputably the further away one gets from the equator. Additionally, migrant studies show that when people move from an area where MS is common to an area where it is rarer they show a decrease in the rate of the disease, whereas migrants moving in the opposite direction tend to retain their resistance to the disease. There is also evidence that susceptibility to the disease might also be linked to the age at which migration occurs. (Click here)
- The female to male ratios of people with MS, which appears to be growing farther apart. In 1940, the ratio of women to men with MS in the US was about 2 to 1. By 2000, that ratio had grown to nearly 4 to 1. (Click here)
- The genetic factors that have been identified as being related to susceptibility to MS, though few, are all associated with genes that play a role in regulating the immune system. (Click here)
- The association of MS with Epstein-Barr virus. Although over 90% of the population is infected with EBV, recent research has shown that people who don't have EBV do not get MS. (Click here)
- According to CCSVI theory, which states that blood refluxing back into the CNS causes the inflammation that is a hallmark of MS, it would seem that the amount of inflammation would continue to increase with the age of the patient. Instead, the inflammation seen in MS typically reaches its apex in the early relapsing remitting stage of the disease, but falls off dramatically when the disease enters the later, progressive stage. Patients who start out with progressive disease (PPMS), though generally older at the time of diagnosis, typically show very little evidence of CNS inflammation. (Click here)
Although it is difficult to understand the above factors in terms of CCSVI, they do not invalidate the theory. MS is an extremely heterogeneous disease, suggesting that multiple factors are likely at work, and that these factors very likely change from individual to individual. In fact, what we call MS may not be one disease, but rather a collection of diseases that share some common elements. A research effort called The Lesion Project (click here, page down to "Heterogeneity of the disease") has identified four distinct lesion types through the postmortem examination of MS nervous system tissues. The project has further found that each patient only exhibits one type of lesion, and that some of the lesion types surround blood vessels while others do not.. This evidence suggests that different disease processes may be at work, and it could very well be that CCSVI plays a major role in some forms of what we call MS, but a lesser role, or no role at all, in others.
This also helps explain the variance in the effectiveness of the liberation treatment from patient to patient. Some patients see dramatic improvements in their condition, sometimes almost immediately after having their veins unblocked. Other patients exhibit no benefit from the procedure, and some even get worse. Dr. Gary Siskin, an interventional radiologist doing the Liberation Procedure in Albany, New York, has publicly stated that one third of his patients see dramatic improvements, one third minor improvements, and a final third no improvements at all.
Dr. Siskin also stresses the importance of doctors managing patient expectations, as the vast majority of materials on the internet (YouTube videos, patient testimonials, etc.) paint an overly positive picture of the results of liberation. This isn't due to any kind of deception on the part of MS forum members or YouTube posters, but is simply a function of human nature. Patients who exhibit dramatic improvements are far more likely to publicize the outcome of their procedures than those who experience disappointing results. It's very important that patients go into venoplasty with reasonable expectations.
The tools and methodology for both the detection and treatment of CCSVI have so far demonstrated sometimes serious deficiencies. On the detection side of things, the most common noninvasive imaging techniques, MRV and Doppler sonogram, have both proven to be less than reliable in identifying the venous defects associated with CCSVI, returning both false-positives and false negatives. Doctors and patients alike have noted that their preprocedure imaging very often does not match up with what is actually found during the catheter venogram procedure, which is the gold standard for imaging venous abnormalities.
The handful of imaging studies done have produced widely varying results, some detecting nearly universal evidence of CCSVI in MS patients, and others finding scant evidence of CCSVI at all. While some of these discrepancies can be attributed to variances in methodology and operator competence, I believe the overall reason for these vastly different findings falls on the failings of technology. So far, the only reasonably reliable noninvasive imaging method appears to be Doppler sonography done according to very specific protocols designed by Dr. Zamboni, but even the results of testing done to these exacting standards at times proves to be unreliable, and, according to the doctor who performed my recent sonogram using the Zamboni protocols, are still somewhat subjective. The physical abnormalities being attributed to CCSVI are hardly subtle, and one would think, given the advanced state of medical technologies, that a variety of instruments and methodologies would be able to pick them up. Apparently, this is not the case, and it is imperative that better imaging techniques be developed, as it is simply not feasible to perform invasive catheter venograms on every patient suspected of having CCSVI.
At a recent CCSVI symposium attended by many of the interventional radiologists most experienced with the Liberation Procedure (click here for report), it was apparent that the Liberation Procedure itself is still in its early infancy and is a very much a work in progress. Many of the presenting radiologists commented on the steep learning curve involved with doing the procedure, and the opinions of these very accomplished physicians varied widely on subjects as fundamental as the proper size of balloons to be used during venoplasty, whether or not stents should be used to prop open blocked veins, and even what constitutes a treatable stenosis. Dr. Sclafani, who performed my attempted liberation (blockages were found but were unable to be addressed, click here for more info) has in no uncertain terms called this an age of discovery. If CCSVI is indeed shown to be a causative factor in Multiple Sclerosis, it's very likely that veins other than the jugular and azygos (such as the lumbar and vertebral veins) play a role in the disease, and presently there is no way to address blockages in these vessels. It's very important that patients be cognizant of these factors when making the decision whether or not to undergo liberation.
Many patients who opt for venoplasty alone (without the use of stents) experience restenosis of their treated veins, necessitating a repeat procedure. If the initial procedure was done locally, and was covered by insurance, this might not pose much of a problem. On the other hand, if the patient traveled thousands of miles, and spent the $10,000-$20,000 often required for travel and treatment, such a repeat performance may prove to be impossible, turning their initial procedure into a financial disaster.
Patients who have stents implanted in their blocked jugular or azygos veins are entering the realm of the unknown, as all of the stents currently in use were designed to be implanted in arteries, which anatomically are extremely different from veins. The only other patient population that regularly has stents implanted in their veins are end-stage hemodialysis patients, who suffer from extremely serious kidney disease. Studies done on the failure rates of these stents are not encouraging, often finding a 50% failure rate after one year (click here for an extensive study, or here for a chart summarizing its results ). I'm certain that the stresses placed on stents during the dialysis process are much different than those placed on stents implanted in CCSVI patients, so the validity of the comparison may questionable. Still, all of the currently available stents were designed primarily for use within the chest cavity, where they are not subject to the constant bending, twisting, and torque that they experience when implanted in the extremely flexible human neck. For patients determined to improve their hemodynamic blood flow and stand a better chance at avoiding restenosis, or whose veins simply don't respond to repeated attempts at ballooning, stents do offer a viable alternative to balloon venoplasty. Clearly, if CCSVI does prove to be an important piece of the MS puzzle (and I believe it will), stents specifically designed for use in the jugulars will be sorely needed.
In conclusion, it has certainly been an interesting 16 months. While much has been learned in regards to CCSVI, there is much more that has yet to be learned. Although some questions have been answered, many more have been raised. A robust treatment trial of the Liberation Procedure that includes sham procedures would be the quickest and most effective way to answer most of these questions. Researchers at the University at Buffalo are currently conducting such a trial, albeit a small one, limited to 30 subjects . Unfortunately, as of today, no other such trials have yet been funded.
CCSVI offers MS patients tangible hope, a commodity in perilously short supply before news of the hypothesis made its way through the Multiple Sclerosis community. Quite literally sick of, and from, taking the drugs that many MSers know are doing nothing to address the underlying cause of their disease, CCSVI has been embraced by patients with a fervor rarely seen in modern medicine. In some cases, I fear that the strength of these convictions has at times overwhelmed reason. I fully understand the desperation felt by those afflicted with this damned disease, as I am subject to it myself. Still, it should be at the forefront of every patient's mind that while the past year has been very encouraging, CCSVI and its role in MS has by no means been proven.
I personally made the choice to attempt liberation because of the severity and aggressiveness of my disease. Each patient must assess their own risk/reward ratio, keeping in mind that many of the questions surrounding CCSVI will likely be answered sooner rather than later, and the techniques used to address blocked veins will mature at a rapid pace, as physicians gain experience and work their way up the learning curve. Quite likely, Liberation Procedures done 12 months from now will be significantly different from those done today, and patients who can afford to wait before embarking on liberation will surely benefit from the accrual of knowledge and the perfection of technique that can only come with time.





![1200351706681[1] 1200351706681[1]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEirWXErVQlcvFBnAjZFjgbOQbwyY9D35n0QA2URpgUOGQg_m0hJvvq16QJ92UpcpnCdFVtWd5PO3BrCCaG0YxqFpLJZoQQOoQquoP96BWbnJVmOPWAvQ76HNkAQknrmkdOynOTimcgRqBs/?imgmax=800)