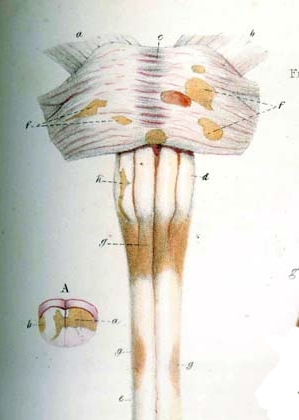
Image via Wikipedia
As most patients know, diagnosing Multiple Sclerosis is no easy matter. Despite sophisticated diagnostic tools and techniques, such as MRI imaging, spinal fluid analysis, and visual and sensory evoked potentials, the diagnosis of MS remains one of exclusion, meaning that other likely diseases must be eliminated before a conclusive diagnosis of MS can be made. There is no test or tests that can definitively determine whether or not a patient is suffering from MS. There are indicators that are strongly suggestive of MS, such as brain and/or spinal cord lesions seen on MRIs, and oligoclonal bands (O-bands) in the Cerebrospinal Fluid, but even the presence of these does not guarantee that a diagnosis of MS is correct.
Although MRIs can detect lesions in the CNS, they can't determine specifically what those lesions are, as a tumor and an area of demyelination can often look much the same on an MRI image. Therefore, a subjective determination of the nature of any lesions found must be made by a radiologist or neurologist. O-bands in the CSF indicate immune activity in the CNS, but they are not specific to MS, as other conditions can also create them. A relapsing remitting course of disability onset is highly suggestive of Multiple Sclerosis, but this too does not rule out other disease possibilities, and some MS patients present with a progressive course of the disease. In the book " Multiple Sclerosis: Diagnosis, Medical Management, and Rehabilitation", neurologist P. K. Coyle writes:
"… early accurate diagnosis is critical. It guides optimal therapy, removes uncertainty, allows informed planning, and improves the patient's sense of well-being by providing an explanation for their problems. Unfortunately, the misdiagnosis rate for MS approximates 5% to 10%, even by experienced healthcare providers"
In an effort to cut down on the number of misdiagnoses, in 2001 a set of diagnostic guidelines was developed, called The McDonald Criteria (click here), that attempts to quantify the test results and clinical presentations necessary for a definitive diagnosis of each of the various forms of MS. In 2009, however, I took part in a study at the National Institutes of Health (the United States government's medical research facility) that was designed specifically to look for patients with Clinically Definite Multiple Sclerosis (more on my experience in the study later). The NIH undertook this study because they had found that the rate of misdiagnosed patients recruited for their MS research studies was at least 10%, and the data from these patients was polluting their research results. The doctors at the NIH were attempting to identify a pool of patients that they were confident actually have Multiple Sclerosis for use in future studies.
There are many diseases and conditions that can be mistaken for MS, including Lyme Disease, Hughes Syndrome, Primary Lateral Sclerosis, Neuromyelitis Optica, Vitamin B12 Deficiency, and Lupus, to name a few. The paper "The Differential Diagnosis of Multiple Sclerosis" (click here) gives a comprehensive overview of the many red flags that doctors must look for when diagnosing MS, and includes a list of 100 diseases that can be misdiagnosed as MS. Another valuable paper on the topic, "Differential Diagnosis of Suspected Multiple Sclerosis: a Consensus Approach" (click here) provides a list of symptoms that should lead a physician to question a diagnosis of MS, and discusses four of the diseases most likely to be misidentified as MS.
If you have reason to question your diagnosis, the above materials can be invaluable. However, be careful not to drive yourself crazy with the information they contain, as they provide so much data that it's very easy to convince yourself that you've been wrongly diagnosed. Even with a misdiagnosis rate of 10%, the vast majority of patients have in fact been given the correct diagnosis.
My own case illustrates the difficulties involved with reaaching a conclusive diagnosis of MS, to the extreme. I had doubts about my diagnosis almost from the day I received it. Although my initial presenting symptom (a slight limp) was very typical for someone with PPMS, the more I read up on the disease, and interacted with other patients who had it (mostly online), the less convinced I became that the diagnosis was correct. I'd been having strange symptoms for years (antibody-based thyroid disease, possible discoid lupus, a variety of endocrine problems ) and my MRIs showed only two lesions, a tiny one in my brain, and a larger, much more invasive lesion at the base of my brainstem. In addition, my spinal fluid results were always normal, showing no O-bands.
As time went on, my disease continued to behave strangely, initially attacking only my right side. Despite the relentless progression of my disability, my MRI images never changed, and haven't to this day. They still show only those same two non-enhancing lesions, which haven't changed in size or shape since they were first seen over eight years ago. My MRI images from 2003 look exactly like the ones I had taken last month, but compared to 2003, I'm now a physical wreck. I switched neurologists one year after my diagnosis, and my new neuro also initially suspected that I might not have MS. I underwent a comprehensive series of tests and scans trying to uncover an alternate culprit, all to no avail. Everything came back negative, and, since MS is a diagnosis by exclusion, the only candidate left standing was Primary Progressive Multiple Sclerosis. So, I was left with the label "atypical PPMS".
Never one to settle for something I wasn't sure of, especially something as important as the diagnosis of a progressively crippling disease, I set about on a quest for second and third (and fourth) opinions. I visited infectious disease doctors who specialized in Lyme Disease, but very specialized blood tests came back negative. I scheduled an appointment at the Johns Hopkins MS center, in Baltimore, and was examined by Dr. Peter Calabresi, one of the biggest names in MS research. He too found my disease presentation strange, and ordered an extensive series of tests, which included the taking of over 30 vials of blood (yikes!), but these too all came back negative. So, Johns Hopkins also concluded that I have "atypical PPMS". "How atypical does a disease have to be before it's not that disease?", I asked to all who would listen, but never really got a good answer.
My primary neuro, Dr. Saud Sadiq, who is himself a highly regarded physician, occasionally sent me for various tests and poking and prodding, just to check that we hadn't missed something. Always, the results came back negative. I kept in touch with Dr. Calabresi from Johns Hopkins, and two years after he first examined me, I sent him some of my latest MRI images, which looked exactly like my old MRI images, and told him that my disease had progressed significantly. As this seemed extremely strange, he asked that I come down for another examination. After another neurologic workup, Dr. Calabresi concluded that he had strong doubts that I had MS, but couldn't figure out what it was I did have. He suggested I might have a mitochondrial disorder, or Sjogren's disease. Off I went to see one of the most noted mitochondrial disease specialists in the states, who quickly determined that my mitochondria were fine. I had a lip biopsy done looking for Sjogren's disease, but, of course, it came back negative…
It was then that I learned of the study being done at the NIH, which cast a wide net looking for MS patients to examine, trying to find a sizable pool of candidates that the NIH researchers could be confident had Clinically Definite Multiple Sclerosis for use in future studies. At first they were reticent to accept me into the study, as they generally weren't taking patients more than a 2 hours drive from their facility. New York City is about five hours from the NIH campus in Bethesda, Maryland, just outside of Washington DC. When I sent them the details of my case, though, the staff became intrigued, and asked me to join the study. In all, I made four trips to Bethesda, and went through every test the NIH Neuroimmunology team thought was appropriate. At first, they too labeled me "atypical PPMS", but in the end, they decided that I most likely do not have MS, as I certainly didn't fit any of the existing diagnostic criteria. They could not come up with a suitable alternate diagnosis, though, leaving me as something of a medical mystery (click here for a WK post I made about this at the time).
Interestingly, the NIH did raise the possibility that my disease could be ischemic in nature, meaning that it might have something to do with my circulatory system. So, I pursued CCSVI treatment, which did show an atypical blockage of my right internal jugular vein. I hate that word, atypical. Instead of the blockage being inside the vein, as is typical and usually caused by a valve problem, stenosis of the vein wall, or an anomalous membrane, my blockage appears to be caused by a muscle outside of the vein pinching it partially closed. Balloon angioplasty couldn't open this blockage, and the use of a stent would be quite dangerous, because the pressure put on it by the muscle pressing on my vein would lead to a high likelihood of stent fracture. I hope to undergo a second procedure some time in the next several months, to look for other blockages and see if there might be a way to address the atypical (ugh) blockage already found.
My primary neurologist says he still can't rule out a highly atypical case of PPMS, though he acknowledges my case is quite odd. Since MS is a diagnosis by exclusion, and we've been able to exclude practically every other possible cause for my condition, I suppose "atypical PPMS" it is. So, I still self identify as an MS patient.
Whatever you choose to call my disease, it's giving me a good ass whuppin'. My neuro and I (okay, maybe just I) have come to an understanding about the label, though: In my case, PPMS stands for the Peculiar Paralysis of Marc Stecker.
How atypical…

I am sorry you have had to join our club of MSers, but am grateful for the contributions you have made and will continue to make during your sojourn with us. And I hope you find soon a positive solution to whatever it is you have.
ReplyDeleteJudy
"Peculiar Paralysis of Marc Stecker" is the best name you could ever gave to your disease. I cannot remember who said or wrote it but giving a name to the origin of pain is reassuring for some people, it is almost if you could grasp some power on it, alleviate it somehow... Unless you have already done so, I would also strongly recommend you read a short story by Tolstoy, "The Death of Ivan Ilyich" Take care :)
ReplyDeleteDid you ever consider you could have a prion disease specifically chronic wasting disease cause that's what I got from taking a supplement called antler velvet spray. Rare indeed I had to figure this all out over a long and arduous 8 or 9 months wasn't tIL I prayed about it that God gave me the answer and he really did no bs.
DeleteThank you for sharing your diagnostic journey with us. I had no idea your particular case was such a complex one. But atypical, as applied to you Marc, is a badge of honor. This is why you stand out in the MS crowd - and we are all better for your contributions.
ReplyDeleteOh yeah. I been where her is at!! :-)
DeleteJust goes to show how unique and special you are Marc! Not typical in anyway. Enjoy today!
ReplyDeleteMarc,
ReplyDeleteI am left with two impressions after reading this. The first is a feeling of regret that you have had to endure this magnitude of testing, poking and prodding, in addition to your ever worsening MS symptoms. The second is gratitude to you that, in spite of all of this, you continue to find the energy and time to share your experiences and knowledge with us. I have learned so much from you in the short time that I have been following your blog.
Thank you once again for all that you do,
Charlie
I just had this discussion with my husband last night...what if I don't have MS and it is something else? Thanks for sharing your journey...gives me a bit of inspiration to push my M.D.s a bit more. I've been labeled atypical as well...isn't the first time in my life I've heard that!
ReplyDeleteI am a fellow "atypical MSer". It really does suck. Thanks for your exhaustive research and willingness to share.
ReplyDeleteKim
Hi Marc,
ReplyDeleteJust came across your blog and wanted to say thanks for sharing your journey!
I'll definitely be back to read more.
Best,
Lauren
Hi Marc, Thanks for another great post. How great to be atypical.(?) I, unfortunately, am about as typical as they come.
ReplyDeletegreat post. I am sure that I fit in the exact category you do. I have never had any type of exacerbation. People do not understand that. Creeping paralysis is truly the best description. It took Betaseron for years, same with methotrexate and I used copaxone for 16 months then I went all the way to Mexico to purchase sf 1019 , well that was a waste of $16,00 there is nothing that has helped me in any degree I have accepted the fact I cannot change the course of this what ever it is, call in MS if you wish but I believe I will continue to call it creeping paralysis because I believe it remains unknown.
ReplyDeleteMarc,
ReplyDeleteExcellent, excellent blog. My husband, who has MS as well, and I enjoy your insights and your work. Paul (my husband) went through the same sort of "What kind of MS do you have?" ordeal two and half years ago. He was even tested for Devic's Disease, twice, and both times it was negative.
It was finally decided he had Progressive Relapsing MS and went for a round of chemo. It seems to have stopped the severe progression but the damage is done. And he will always be in pain which is something we feel the neurologists need to address more openly. He had one neurologist who didn't believe he was in pain whatsoever. Paul immediately switched doctors and this neurologist, who he's been with for three years, acknowledges the neuropathic pain.
Thanks again for your work.
-Margaret
who ordered the chemo treatment, I've never heard of that option. For how long? It stopped the progression for good? please respond, have a lot of questions, what area of the country are you in? thanks
Deletemarc
Marc, you are responding to a comment that was left back in 2011, so I'm pretty sure you won't get a response from the original commentor. I don't know what kind of chemo her husband underwent, but chemo is very rarely used on MS patients these days, primarily because of the high risk of side effects.
DeleteIf you are experiencing relapses and/or have enhancing lesions on your MRIs, you should consider looking into HSCT, a type of stem cell therapy that first oblates the immune system using chemotherapy drugs, and then reboots it through the use of a stem cell infusion. If you search for "HSCT" in the search box on the upper left-hand corner of this blog, you'll find several blog posts about this treatment…
You might also want to research "intrathecal methotrexate" using the same search box. This is a treatment used by a few neurologists, my own included, that has shown some promise in slowing down progressive MS. The vast majority of neuros are very reticent to try this, though…
DeleteWhat is MS? WIll the medical community ever really know? Ms, lymes, devics, whatever it is they all suck and since nothing has been cured since Polio I am not holding my breath. Its a great opportunity for someone to make a ton of money off the randomly selected ranks of we pwms. When I read my neuro's reports I feel he thinks I am creating these symptoms emotionally since I have negative o-bands and my mri lesions hae not changed nor have they enhanced since diag 5 yrs. I have deteriorated in a very short time. I would love to swith bodies with the asshole for just one day..
ReplyDeleteWhat I don't see in your commentary are thoughts about the limitations of MRI. Even the strongest magnets and best software do not accurately depict the CNS. They tell us next to nothing about the gray matter, especially.
ReplyDeleteSo if your disease is clearly progressing but your MRIs remain unchanged, why not chalk that up to the failure of technology rather than putting the cause into question?
PPMS is notorious for low lesion load in some persons, and that may be because it is much less a disease of inflammation than other forms of MS. There could be much more direct axonal degeneration, not so readily identified by technology.
I understand you strong need to know--that's a very normal human response. Sometimes, though, pigeon-holing just isn't possible. And even if you were classic for PP, that wouldn't accomplish anything in terms of treatment.
I have RRMS, undiagnosed for 10 years at least, because radiologists looked at my age and MRIs (the sum total of what they knew about me), and decided I had microvascular ischemic disease. My MRIs were a mess, but 'atypical.'
I am more and more convinced that MS itself, and all its categories, represent a rough grab-bag of similar but distinct disorders. Labeling doesn't accomplish much, except maybe for drug manufacturers.
Thanks for writing this Marc! Another great and valuable post!
ReplyDeleteI just really hope that solutions can be found for you, and for all people fighting MS (or whatever it is!?). If you undergo a second procedure, I hope you have good results-- wish you the very best!
ReplyDeleteprairiegirl
If only Dr. Gregory House and his team were real!
ReplyDeleteMultiple sclerosis (MS) is a nervous system disease that affects your brain and spinal cord. It damages the myelin sheath, the material that surrounds and protects your nerve cells. This damage slows down or blocks messages between your brain and your body, leading to the symptoms of MS.It may be an autoimmune disease, which happens when your body attacks itself. Multiple sclerosis affects women more than men. It often begins between the ages of 20 and 40.
ReplyDeleteGreat blog. when I went in for my second opinion at a major MS center in Boston, after a number of tests, the MS specialist said that she was 98% sure I had MS...the only way to be 100% sure was to do a brain byopsy...I politely declined.
ReplyDeleteGreat blog Mark. I guess I can somewhat identify with your feelings. A part of me is still unwilling to think that I just have MS. I was dx'ed 27 years ago (5 O bands and elevated IgG synthesis rate and MBP). Then I was asynptomatic for 14 years and then a slow progression that started in 1998 with a more rapid progressiom since 2009). Nice to know that MS is not the only disease that has O bands. To my knowledge, none of the MRIs (first one in 2006) I've never have had any enhansing lesions. Stented azygous and IJV (thoracic cavity) at Stanford in 2009. No Chiari mri evidence even though I do have symptoms. But I'm glad I don't need decompression surgery. I do have quesions since I have a 23 yo daughter that had postpartum optic neuritis as did I 27 years ago. A sister that had psuedotumor cerebri. At least the neurologists in my "neck of the woods" look at you like you have a third eye in the middle of your forehead if you raise questions. I also didn't seem to follow the RRMS route that the majority of MS patients seem to follow. Just looking for some answers. Hope you get some answers too.
ReplyDeletedear marc
ReplyDeletei read your post and was very identify with your conflict since i'm ms too (10 years diagnosed and 10 years withour diagnosis) and i lost faith on the doctors attitude about ms. i have also a very interesting case, i still don't know if i'm like, you said Peculiar Paralysis of shoshi shaffir, i tend to think that if so many are like us, maybe the whole idea of doctors thought about ms is mistakenly wrong?!
shoshi shaffir israel (age 56) shaffir51@gmail.com
My MRI IMAGE has not changed for going on 7 yrs. and the couuntless neuros say, I too the dr's say have ATYPICAL MS.
ReplyDeleteYou could have written my journey. I also present as "atypical.?"
ReplyDeleteMany brain lesions, no spinal, no o bands, no evoked potential confirmation, but mobility and fatigue problems.
I have to say Thai I have never read anything by someone who I so much identify with.
Thanks.
I too presented with some atypical symptoms and went through numerous tests. My MRIs have been "stable" for a few years and only when I apparently ticked off my first neurologist after complaining of intense pain in my legs he told me I did not have MS and find a new doctor. He informed me I did not have MS because MS did not hurt. I was finally told I have Susac Syndrome because I have a significant hearing loss. Who knows what Ihave at this point.
ReplyDeleteI was diagnosed with MS 12 years ago, 3 months after the birth of my first son. My symptoms were right optic neuritis, slight foot drop, fatigue and hip pain in the AM. I had two brain leasons and elevated IGG levels in my spinal fluid. The symptoms resolved 3-8 months later and I have not had any symptoms since nor did I start the ABC drugs. I had similar symptoms 6 years earilier. Both times that I had symptoms I was taking Depo Provera and believe this was the initiator of MS like symptoms. It is impossible to carry individual health insurance as I have been tagged with MS now. I am currently three months pregnant with my second child and worry that the symptoms will reappear after delivery. There is a proceedure called the obliteration proceedure for treatment/cure of MS symptoms which I plan to be tested for after delivery. Thank you for your article from which I can relate and find hope in.
ReplyDeleteHi Marc,
ReplyDeleteI read the NYTimes piece recently, which left me wondering....how often is MS diagnosed when it's really something else.
I read through your details above and was struck by this:
Instead of the blockage being inside the vein, as is typical and usually caused by a valve problem, stenosis of the vein wall, or an anomalous membrane, my blockage appears to be caused by a muscle outside of the vein pinching it partially closed. Balloon angioplasty couldn't open this blockage, and the use of a stent would be quite dangerous, because the pressure put on it by the muscle pressing on my vein would lead to a high likelihood of stent fracture. I hope to undergo a second procedure some time in the next several months, to look for other blockages and see if there might be a way to address the atypical (ugh) blockage already found.
When I hear of tight muscles (presumably), I think magnesium deficiency. So "simple" most neuros and other specialists never think of it. Yet, most of us are deficient. And some of us very deficient. Especially if we've over-consumed dairy, especially as children.
I searched your blog for "magnesium" yet nothing turned up.
I know it must get tiresome, strangers saying, "have you tried this or that?" But the science is behind this suggestion, it can't hurt you, and it's cheap.
Good luck,
g
I can completely understand, Marc - I've been suffering increasing disability for over 13 years now - diagnosed with MS in June 2012 and again in November 2012, only to have a new neurologist suggest my symptoms are psychogenic because my many lesions are 'tiny'
ReplyDeleteWishing you Peace and Sunshine
I went to a surgeon for a herniated disk. He wanted to do more MRIs to look forextreme Ms. He didn't tell me I had it but said he would do a lp during the surgery to look for it. I found out later he had diagnosed me with extreme ms but did the surgery anyway even though it could have made ms symptoms much worse. So I had back pain I could have lived with now I can't walk. I am at the end of my rope and don't know what to do. I Still haven't had a symptom of ms as they've been described. And im stuck in the fl keys. The newer mri's show lesions that are smaller or have disappeared. The 20 or so doctors I've seen just give me the runaround. All I feel is severe pain in my back but they don't think that's from cutting my back open and screwing around with it. I think doctors are idiots but I was too for trusting them. What now?
ReplyDeleteAnyone with mystery MS or atypical MS have a Thailand connection before your brain lesions appeared?
ReplyDeleteDo you feel confident you don't have Lyme? Infectious Disease people don't believe Lyme is an epidemic. The CDC has it's head in the sand about the severity of Lyme disease. Did you get a CD57 test? Follow up with a Lyme Literate doc? Good luck.
ReplyDeleteThanks for the advice, but I was thoroughly checked by two of the most prominent Lyme literate doctors in the Northeast several years ago, and had my blood tested by a lab specializing in detecting line and other tickborne diseases. Unfortunately, all agreed that I do not have Lyme.
DeleteVery interesting reading! I too, was diagnosed with RRMS in 1993, by a local againg neuro; refuse to go see him again, not appreciating his bedside manner. I have never taken any prescriptions related to MS, refused to enter a study at UBC, as I was witnessing my brother (16.5yrs.my senior), wasting away from PPMS. At the time, he suggested I keep doing what I already doing, ie.alternative therapy! I have stuck by that protocol for years now, until recently my syptoms have deteriorated to the point that I now use a cane, occaisionally a wheelachair, depending on leg function. Just this past fall I approached a local naturopath to receive Meyers cocktail IV's, he then suggested trying Lyme testing....I was very skeptical, as I had been seeing a local, very well recognized, live blood analyst for the past 17-18 years, who was adamant that I DIDN'T have MS, but another type of sclerosis! I was quite sure that he would've detected LYME & asked him point blank, to which he said NO, I didn't have Lyme, no chance.
DeleteSeveral months later, not having anything to lose, except $$$, I requested the test....lo and behold, it came back positive, through testing confirmed through IGeneX in PaloAlto, CA.!!!! Upon seeing the ND, he suggested LDN (low dose naltexone), I take 3mg at bedtime and have added CBD incture & THC oil, both products of marijuana for sleep! I start Lyme treatment this coming Tuesday, Jan.12th. It will be a long arduous road, but I'm up for it....will keep you posted..... I live in a small town in the interior of B.C., Canada, and we are very luck to have a local Lyme literate pharmacist & naturopathic doctor in our town. As well the pharmacist says she knows of only two other Lyme Literate MD's practicing in a nearby community.
Hmmmm, the mystery continues....Cheers, moving forward :))))
I have been reading your blog for some time now. My story is different in that I have 11 O-bands, two small brain legions not typical of delimaniting disease, unexplained symptoms for over 6 years. Originally dxs was MS, since then with no changes on MRI dxs was removed. Have gotten 2nd, 3rd and 4th opinion from Mayo Clinic in AZ. I have had every test from Lymes to NMO to everything else to many to list. Perhaps someday all the people we read about will finally have an accurate dxs and treatment to stop the suffering that so many of us undiagnosed people have. Best wishes to you and your journey.
ReplyDeleteJeez I thought I thought I was the only one with a concern that I might be misdiagnosed. I was diagnosed three years ago woth adem and them relapse remittance ms, within one week!! Some of the lessions dissapeard and some had gotten smaller. I am not on any meds and don't have any of the ms symptoms!!
ReplyDeleteIt's always important to get a second opinion, especially if the doctor's diagnosis doesn't seem to be matching up with the symptoms. No one can go back to a physician afterwards and tell them to replace years of their life. Years that were spent treating the wrong disease or getting worse because the true cause of their symptoms was not addressed.
ReplyDeleteI think doctors can miss things sometimes and some diseases closely resemble each other. It's better to be on the safe side if a test is inconclusive.
I had lower back surgery because of a limp and back pain. Since the surgery I still have the same herniated disk that they were suppose to fix and back pain so severe I can't walk. I'm stuck in s. Florida being told to get over it you have ms. Never had any symptoms of ms. Still don't believe it and I can't get any help. Ms was a good excuse for the incompitance
ReplyDeleteHi Mark,
ReplyDeleteTo inform you; i underwent a upright MRI and there were 2 compressions of the spinal cord. i'll visit a neuro surgeon soon.
Following is a translation from the dutch neurosurgeon site, for the first time i recognized my symptoms....
===
Cervical stenosis (narrowing of the neck)
Download as PDF
Narrowing of the cervical canal is like the narrowing of the lumbar spinal canal and can often then give rise to complaints.
Anatomy
(it's not the full text, that's too lon)
The signs and symptoms of cervical canal stenosis are the result of the tribulation (compression) of the spinal cord and / or nerve roots. One can imagine the pressure on the spinal cord causing direct mechanical damage them, especially if it happens repeatedly during movement, but more likely it is that the circulation of the spinal cord is disturbed by the flattening of nourishing blood vessels. The spinal cord can become thereof damaged, myelopathy (myelum means spinal cord) is mentioned. In the cervical spinal cord motor running long jobs, which are the nerve fibers that bundles the missions of the big brains pass to the cells in the spinal cord that control the muscles. Spinal cord also contains the long sensory pathways, these bundles of nerve fibers that entered in the spinal sense stimuli to the brains. When affliction of the spinal cord will therefore motor and sensory disturbances occur contained herein that patients express the movements of their legs no longer have control and lurching walk. On the one hand, this is because they have less power in their legs, (this is called a paralysis or paresis of the muscles), on the other hand it is also because they feel the position and movements of their legs less. In addition to a reduced position feeling, there is also a diminished sense of touch. By decreased sensation in the feet may appear they tiptoe while they have no stockings. In addition, the power reduction of spastic paresis or nature, that is to say that in spite of the reduced force the legs are weakened, but rather more rigid than normal so that it appears as if they stick to the ground. In addition to a disorder of the motor and of the feeling in the legs can also exist for urinary incontinence, that is to say that the patients do not have their urine bladder under control and at inopportune moments, can lose urine. Another phenomenon that sometimes occurs, is a sensation of electric current goes through the spine when bending the neck. These are all signs of affliction of the spinal cord. If the myelopathy progresses and the pinching of the spinal cord is not removed, it may result in a total interruption of the spinal cord, called a spinal cord injury that is characterized by complete paralysis and numbness of the body part below the level of the damage.
The signs of compression of the cervical nerve roots, also radiculopathy (radix meaning root), consist of shooting or radiating pain in the shoulder or arm, possibly accompanied by numbness or tingling, which aggravated or may be by bending generated or turning of the neck, or by stretching the arm.
The symptoms of cervical canal stenosis therefore very similar to those of the neck hernia, which is not entirely surprising, since both conditions can lead to compression of the spinal cord and nerve roots. Rise The emphasis is on the stenosis more on the pinching of the spinal cord and the neck hernia more like the roots. One difference is that the stenosis symptoms gradually commit to act, while complaints may arise as with thunder. Acute in the neck hernia Naturally, the cervical canal stenosis and neck hernia also combined, as often happens. For the uninitiated, the signs of the cervical canal stenosis resemble other spinal cord disease, such as multiple sclerosis. Therefore, neurological examination and imaging tests required to arrive at the correct diagnosis and to set the appropriate treatment.
===
regards,
Robert
(Robnl on thisisms.com)
Hi Robert, thanks for your comment and suggestions. Unfortunately, I recently had a thorough workup looking for signs of stenosis, or even spinal cysts, but none were found. So, I'm still in that "mystery" category.
DeleteMy grandmother suffered from spinal stenosis, and her symptoms did look eerily like mine. Unfortunately, she never had the surgery that could alleviate her problems, and towards the end of her life she was a quadriplegic.
Definitely valuable information, thanks for passing it along
I am a mystery since late 1980s leg pains,fatigue,headaches,vertigo(debilitating). Had a positive lyme test did IV anibiotics then got severe fatigue too tired to go to bathroom 5 feet away and pain in every joint. Mouth sores, vertigo and leg pain numbness cold feeling progressing up both legs joint pain fatigue continue,raynauds, hair loss, The pain in my legs is neuropathy but why? and progressive like CIDP but pain more than real paralysis though weakness and pain go together.Now have severe shortness of breath just doing small activities. Too tired to do dishes or even shower. I've been treated for lyme many times but not specifically for bartonella or babesiosis which my symptoms are like. I had 3 children had pleurisy after second child. My oldest is starting to have similar symptoms. Mother has lupus we think depends what dr you ask! I have negative ANA. Encephalopathy on spect scan and abnormal EEG. ?small fiber neuropathy on punch biopsy. Oh and I get fevers sweats and chills especially with antibiotics? herxheimer? I am a nurse and cannot work anymore and need a diagnosis. Any thoughts? vertigo comes and goes not as bad as in 1996. legs and fatigue are main issue almost fall a lot and always to the left side.
ReplyDeleteSo sorry to hear about your problems, Elsa. Wish I had some suggestions for you, but I'm afraid that many of us test the limits of medical knowledge. Based on my experiences, there is a wide range of illnesses out there that haven't been properly identified, and patients are often given "garbage can" diagnoses just to satisfy both the doctor and patient.
DeleteTry not to give up, and keep searching for answers. At the same time, try not to let the situation drive you crazy. Easier said than done, I know…
Hi,
ReplyDeleteCame across this blog and was very interested in your journey.
It has been suggested by my family doctor, neurologist and MS Specialist that I have MS.
I am 49, female, enjoy farming life, married with 5 children...life is very busy.
To be diagnosed with this about a year ago after a flotilla of MRI's, blood tests, appointments has been quite life changing. Taking time to enjoy a bit slower life and take things a bit easier have been forced upon me a little earlier than I expected, but life is really wonderful.
My initial MRI revealed a lesion on the spinal cord at c6 and c7 level...the discs were bulging towards the spinal cord. I hadn't had an accident to cause this...just a lot of heavy lifting over the years and wear and tear. I have had no lesions on my brain at all.
My blood tests at the time revealed my stored iron levels to be extremely low - 3 - when they should have been 15...so I had deleted my iron stores. My other bloods were good...no infection, no nasties.
My symptoms were severe headaches(migraines), acute neck pain, tingling in my arms and hands(especially when I extended my neck forward), a bit of nausea, photo-phobia(dislike of brightness) and fatigue.
I went to see a neurologist who said I needed to have my neck fused or I would become a paraplegic, and then I went to see a neurosurgeon who would perform the operation. He put me through strength tests and reflex tests and balance tests.
I passed all of them. He told me plainly that if I changed my lifestyle, took it easier, I would give my neck a chance to heal itself. He said he could make me worse with the operation. He recommended a book to read - heal your own back and neck by Dr. Robert McKenzie, a New Zealand Doctor.
So I opted for the life change. I stopped mowing lawns and driveways, ceased chopping wood(which I loved to do) and changed how I lifted things and how much I lifted. I quit my casual job as a Personal Care Assistant and concentrated on getting better.
After a year of consciously changing my work habits and taking a certain iron tablet/diet that doesn't cause constipation, I got my stored iron level back to 17 and the tingles that drove me crazy for about 6-8 months have all but gone( if I overdo an activity I can get a tiny tingle in my hands, but it usually goes away).
I had a spinal tap in Dec last year and there was something wrong with the 0 band(sorry I don't know much about this bit!). Then I had a follow up MRI and there were no new lesions other than a teeny one near c1(the MS specialist when he looked at the MRI said he wasn't convinced it was there).
I also have an old injury in my lower back at L4 and 5 from 13 years ago, but I have learned to manage the pain...anyway, it flares up now and again and last month I have had numbness in my lower legs and feet(both).
Of course my doctor says it is a classic MS symptom, but I know I have been using my lower back more lately and personally think it is just nerves acting up because of being pinched.
Or maybe I'm just in denial!
I have another MRI coming up in November so will see how I go. The MS Specialist wants me to go on a drug called Gilenya...I'd like to try to stay away from any drugs if I can until I know for sure. I have also been taking B12 lately and feel a lot chirpier.
Ah well, that's my story...has been good to tell someone actually that may relate.
I hope this finds you well...keep smiling. :-)
Hi ... I just came across your post after questioning my PPMS diagnosis ... I haven't yet had a spinal tap but MRI's and symptoms have led to my dx... What baffles me is the amount of neurodegenerative diseases there have been in my family but each one is different! ... What I wonder now is if my family were misdiagnosed (parkinsons, alzeimers, spina bifida, schizophrenia and tourette tics and my father is now due a brain scan)... It is all one big mystery to me...
ReplyDeleteHi Marc,
ReplyDeleteand thanks for a wonderful blog. Has there never been anything "wrong" with Your spinal fluid (elevated igg etc.)? I have been having severe PPMS-like symptoms for the past three months after an influenza/respiratory infection. Clear mri:s and clear lp (although O-bands were not checked for some odd reason).
Mika from Finland
Hi, no, there's never been anything unusual found in my spinal fluid. I do have markers for inflammation, but that's about it. No elevated antibody levels, no O-bands. Sorry that it sounds like you're in the same boat. Seems to make it all that much harder not knowing exactly what's afflicting you… Wishing you the best…
DeleteHi, and thanks for your answer. You referred to markers of inflammation in your spinal fluid. What kind of markers were/are they, if I may ask?
ReplyDelete-Mika.
My neurologist has his own laboratories, which do some proprietary screening of cerebral spinal fluid. The markers I was referring to are osteopontin and fetuin-a.
DeleteSo basically elevated protein levels in CSF?
Delete-Mika-
Yes, but specifically those proteins, which my neurologists lab has identified as potentially important markers for MS.
Deletei have all ms symptons but recently had c6 c7 facetectomy 2011 had c4 c5 disc replacement both began with severe headaches i suffer with tingling numbness pains around chest like heart attack symptons vision blurry very poor eyes constantly watering bladder incontinence bowel prolapse can i have MS ?
DeleteCan't really even take a shot at a diagnosis, as I am not a doctor. It does sound, though, like your doctors think that your problems have to do with Cervical Spine troubles. There are many, many conditions that can present with the symptoms you describe. My best advice would be to seek further professional opinions if you are not satisfied with the care you have already received.
DeleteHi Marc,
ReplyDeleteYou have an interesting blog and it is always so entreating to read others "complicated" stories of the neurological forest. I´m a weird case myself but I have a very slow progression. I saw that you have a negative spinal tap, as have I. I also have a negative VEP but I have many small (biggest about 5mm) lesions decorating my brain (periventricular- mostly), a total of 30-40 are seen on 1,5 T MRI. No spinal lesions. I have no diagnoses, because I´m not typical "anything", everything has been ruled out. At this point I would rather like to be "misdiagnosed" with MS than having no help or medical attention. My symptoms are not seen or felt easily, so it makes me feel alone in my twitching/tingling world. My symptoms are all over. I told my neuro before I got the MRI done, that I knew there were small lesions all around in my brain. Because I can feel how like "this nerve is not getting it´s message right today, or for this week, or month, or never again". And I was totally right, small lesions all around. But the thing is I don´t have anything "to go with it" to get a diagnoses. I don´t really care if it is MS, just that they would find out what is eating up my brain! They say, while they can not prove it is MS, then they can´t really admit that the lesions are the reasons for my "everything". So I´m stuck in the land of limbo :-/
But I was thinking, when reading your story, that there must be also unseen lesions in your brain. If you would like to read my story, then here it is: http://www.medhelp.org/user_journals/show/1064799/My-never-ending-story-up-to-date-?personal_page_id=2173875
My best wishes for you,
Dagun
Thanks you... you save my life today.
ReplyDeleteThank you... you save my life today, and put words on my pain.
ReplyDeleteI have so much respect and gratitude to that, in spite of all of this, you continue to find the energy and time to share your experiences and knowledge with us
ReplyDeleteHello,
ReplyDeleteI am 46 yrs old male and I have been told back three years ago in march I have COPD, Ephemmiza and Aspergillous, than in oct 2013 lower vule block surgery. Now this year in march 2015 had to have appendix removed. Now these days I am going through having to use a cane, walker or wheelchair. Because for reason now my legs are tingling and I get tired with pain at times. I am now in an Adult Forster home just two years ago I was able to walk, doctors are looking for MS first MRI with contrast came back negative on my brain, this Wed I will go for MRI on my neck and Spine. All blood tests negative so far, went to my Doctor this past Friday he told me MS can appear in neck as well in back without signs. I have support from church, family and friends although I am not sure about where this will go.. Thank GOD I can enjoy life although as my health troubles allow me.. I get as well back of head headaches sometimes to the point I can not lay. Guys I am wondering is there something I am not asking, plz I am scared
Gary
Hi Gary, so sorry to hear of your travails. MS can be an incredibly hard disease to diagnose, as so many other illnesses can show similar signs and symptoms. Getting MRIs done of your cervical and thoracic spine are a definite must, as progressive MS can often show itself in the form of spinal lesions. In fact, some forms of progressive MS have in the past been called "spinal MS". You should also make sure that you see an MS specialist to make the determination of your diagnosis. I know firsthand that many general neurologists simply don't have enough experience with the disease to get the job done correctly.
DeleteWishing you the best, and hoping that you find some answers…
I am looking for a little advice from anyone. Here is my story. In 2011 while on leave from the Marine Corps I was hunting in Pa. It was then that I first noticed a sharp pain when I moved my right eye. Upon returning home the pain remained and I found four or five ticks on my body. Over the next few days my vision started to worsen so I went to medical in Bethesda MD. After excepting the fact that I was not faking to get out of deployment a LP was performed. A few days later I was contacted by phone and diagnosed with MS. Now a few years have passed and I have since been retired from the MC due to my illness. I have been thinking is it possible that Lyme Disease was actually miss diagnosed for MS. If so what test should I request. I may just be grasping for straws here but I'm just keeping hope alive. Any insight is appreciated.
ReplyDeleteI'm surprised they would diagnose you with MS based on a lumbar puncture alone. Was no MRI performed? It certainly is possible for Lyme disease to be misdiagnosed as MS, but I think it would probably take more than a few days for the neurologic symptoms of chronic Lyme disease to show themselves. However, I'm no expert. In order to definitively rule in or out Lyme disease you need to see what is known as a "Lyme literate" Dr., which isn't the easiest thing to do as most mainstream doctors don't generally acknowledge the seriousness of chronic Lyme disease. I suggest you check out the Lyme disease networks website and visit their forums, where I think you'll find people who can direct you to the appropriate physicians. These doctors will send your blood samples to laboratory specializing in the detection of chronic Lyme disease, tests that most testing facilities don't conduct. Here's the website link:
DeleteLyme Disease Network
Great Blog, thank you Marc for sharing your experience.
ReplyDeleteAdd me to the list of Limbolanders. I've been in DX limbo for 4 years. All MS testing was performed, MRI's Cerivcal/Thoracic/Lumbar, Lumbar puncture all negative. Brain MRI suggestive of MS or small vessel disease. Evoked potentials done. VEP was abnormal (which is the one they use to compliment a diagnosis of MS). All other diseases (to my knowledge) have been checked into and have been ruled out. I continue to be monitored by my neurologist with yearly MRI's. They have all come back showing no changes or abnormal enhancement.
I have many MS-like symptoms and currently on FMLA at work because I'm so sick I can't make it in most times. I asked my neuro why I have not been dx with MS yet if all other diseases were ruled out. He said I need either one more lesion or an enhancing lesion for an official diagnosis.
In the meantime I will probably need disability at some point but have no diagnosis to support it. :(
Yup; me too...going on 5 years without a diagnosis. Been to 4 Neuros, 3 of them MS Specialists
ReplyDeleteWon't even go into the details; it would be a novel. Seriously.
Suffice it to say that the last MS Specialist at NYU said I'm a "...very unusual and complicated case..." and that he doesn't get stumped often.
Lucky Me
Lucky Us in Limboland
Hi Marc, I'm so glad I came across your blog! I've been rapidly declining for the last 11 months and despite 11 O bands, abnormal VEP in both eyes, and hemiparesis on the left side, I have no visible lesions in my brain, c spine or t spine. The two neuros (one an MS specialist) have been hesitant to DX. They've repeated the MRIs multiple times this year (14 MRIs so far), but no lesions. They checked Lyme, paraneoplastic, and a slew of other outliers. MRA showed no abnormalities.
ReplyDeleteA year ago I was jogging with my dog, now I walk with a cane and struggle with every day tasks. I'm terrified they won't figure out how to treat me before I become seriously disabled.
Hello,
ReplyDeleteJust wanted to get some opinions on whether or not to start with a disease mod med. I'm a 50 year old female and was diagnosed with RRMS in May 2014 solely based on my brain MRI showing about 12 small lesions and symptoms (dizziness, fatigue, excessive sleepiness, and ringing in ear) which all lasted about a week and never came back again to this day except the excessive sleepiness which has stayed with me the whole time, but I'm on meds for it and it helps.
Negative LP (no O bands), no lesions found on spinal MRI, Negative neurological exam, 0 on estimated disability scale, none of the typical symptoms of ms (no numbness or tingling anywhere, no optic neuritis, no urinary problems, no pain etc). They've also ruled out other mimics, as far as I know.
Since diagnosis, I've done numerous MRI's and nothing has changed, no active lesions and still showing the same number of lesions.
During this time, I've also seen 3 neuros (for second opinion) specializing in MS, 2 of which told me that yes in fact I do have RRMS, and the 3rd said no I don't have MS.
So, not sure what to do at this point. My current neuro (one of those who diagnosed me with MS) wants me to get on a med, but I'm not sure if want to based on my uncertainty. Any thoughts?
Thank you in advance :)
Hi, please keep in mind that I am not a doctor, so I'm really not qualified to hand out medical advice.
DeleteThat said, I am a very experienced patient, so I'll tackle your question from that perspective. If I were you I would first try to get some kind of definitive diagnosis. I know that you have already tried three doctors, but there are so many diseases that can mimic MS that getting a diagnosis can take quite a long time, and may require visits to numerous specialists. The fact that you don't have any enhancing lesions or O-bands would indicate that whatever you have is not currently in an active inflammatory phase. Keep in mind, lesions as seen on an MRI only indicate areas of concern, they don't tell whether the lesion is demyelinating, ischemic, or something else.
It's generally thought that the misdiagnosis rate in MS patients is between 5%-15%. So, you certainly could be misdiagnosed.
As far as whether or not to go on a medication, in your case that would be a tricky question. Unlike many other MS advocates on the Internet, I am not opposed to the current crop of disease modifying drugs, as I know far too many patients who have benefited from them to condemn them wholesale. They are far, far from perfect, and do nothing towards curing the disease, but for some patients they do dramatically increase quality of life (albeit at the price of worrying about possible serious side effects).
The growing sentiment among MS doctors and researchers is that early intervention with highly effective drugs can help keep the disease at bay for as long as possible. So, if you had a definitive diagnosis of MS, I would probably recommend you go on a drug. Since your diagnosis is up in the air, though, in your case is a difficult question, made even more difficult because all of the available drugs work by either modulating or suppressing the immune system, and judging by your lack of enhancing lesions and O-bands, it doesn't seem like your immune system is currently involved in exacerbating your disease.
Wish I could give you a better answer, but at some point I do think you need to trust the judgment of your Dr., as long as he's a doctor you can trust. You say you were diagnosed with RRMS, but it doesn't sound like you ever suffered from relapses followed by remissions. In that case, if you do have MS, it could be of the progressive variety, for which the current drugs don't do much for the majority of patients.
Again, if I were you I think my first priority would be trying to seek more answers. That may mean trying to go to a major MS facility (such as Johns Hopkins or the Mayo Clinic here in the states).
Wishing you the best…
This was a very interesting blog. I am now going through a very similar struggle. Brain lesions that haven't changed in 3 years yet I continue to deteriorate. My doctor believes I have MS but my spinal was normal and my back and neck mri showed lots of problems but no lesions. Just had a VEP and awaiting those results, the tech said it looked normal.IM at my wits end as I see myself deteriorate with all the othe issues I deal with llike endocrine issues, hashimotos thyroiditis like you have, insulin resistsnce, pcos, vitamin d deficienCy, my other dx. I think I have 20 dx. I keep searching for answers. Thanks
ReplyDeleteI am suspicious I have MS esp because I have Crohns disease which is related. I feel I have very many of the symptoms, esp the gait.I drove to work (of course my 1st day there ) got out of the car and could not walk. My legs kept jerking and my brain would not let me walk, I almost fell down before I got to the door. I had to hold on the the counter but my arms and body kept jerking and swaying into circles. My boss tried to put me in a chair but I fell down and cut my wrist. So they called an ambulance. I couldn't remember words,understand words, was pausing in between words, repeating words..The EM ran a CT scan and blood work, urinalysis. All negative.But would not do any other testing because I have no insurance. Because I was stable and not critical, they said to go get a walker and sent me home. My legs were still scissoring and I was still stumbling. I kept asking them if I had insurance what would they be doing? They evaded and did not give me an answer. My discharge paperwork called it muscle spasms. Really? Yet he recommended a neurologist. I had to repeat what happened,my symptoms, medications to 4 different people (Fire Dept, paramedics, nurses in ER then ER Dr) that my brain just would not tell my legs and my mouth what to do. I also told them that I did not have a headache but my head felt swollen on the inside. This was obviously neurological. I tried to just have a consult but no neurologist will do that without insurance.I couldn't go to work today, I was still very weak and sore from my legs jerking for 8 hours.Praying this wont ever happen again. I have an appt with my primary on Friday so maybe he can help me figure it out without an MRI ($3K to $5k) If my primary suspects MS can he even treat without confirmation? I am glad I have been reading this post because I thought an MRI or spinal tap always confirmed MS, but have read here that is not always the case.
ReplyDeleteHi, I'm awfully sorry to hear about your medical condition, as well as your predicament regarding medical insurance.
DeleteAlthough I am not a doctor, it doesn't sound to me like what you're describing is Multiple Sclerosis. Of course, MS can present itself in many different ways, but what you are describing sounds more like a mini stroke (also known as a TIA) or perhaps some sort of seizure.
It is imperative that you do see a neurologist given the symptoms you describe. I know this may be very difficult since you don't have medical insurance, but perhaps your GP can suggest a charitable organization that might be able to assist you with the costs.
I hope you don't mind my butting in a bit here, but if you don't have medical insurance you really need to look into getting some under the Affordable Care Act. Perhaps this might go against your politics, but don't cut off your nose to spite your face. Under the ACA, you should be able to sign up for low-cost insurance with no preconditions, and might even be able to get a subsidy to help pay for it. Unfortunately, I believe the sign-up time has passed for this year, but there may be some way to get around the deadline. It's definitely something you should check into, either through your state exchange, or, if your state doesn't have one, through the federal exchange.
Having health insurance in the USA is absolutely vital, as I'm sure you are all too well aware. I hope your general practitioner is able to get you a neurologist to give you a thorough exam, including any radiology tests necessary to make a diagnosis.
I'm very sorry that you had to suffer through all of this, and I understand how frightened and confused you must be. All of my best wishes are with you…
So glad I found your page...I was first diagnosed about 4 years ago, but they started testing me 6 years ago. We/they ruled out a bunch of things then told me I have MS, but no one could definitively say what kind. After many MRI's, tracking disability, and a consult with my hematologist they confirmed Relapsing Progressive Multiple Sclerosis. Apparently because I have an extreemly rare blood type it may have played a role.
ReplyDeleteThis comment has been removed by the author.
DeleteMiriam, your situation does sound very complicated. In some MS patients lesions can "heal", but usually only early in the disease course. I completely understand and empathize with the difficulty of your situation, as for people with progressive neurological disorders there are many, many diseases that share lots of common symptoms and diagnostic markers. I, too, suspect that my initial neurologic problems were caused by a one-time "attack", and that the progressing disability is due to some process that is not yet understood. All I can say is hang in there, new discoveries are being made every day, and hopefully one of them will benefit us…
DeleteThis comment has been removed by the author.
ReplyDeleteThank you Marc for putting all this craziness in perspective. I had been to 7 doctors before my current decided to run tests for fatigue.I had a chronic throat infection this January then developed pins and needles and numbness in right arm and a limp about 6 weeks later,next the mental confusion set in couldn't do basic mathematical tasks put it down to just being tired, then the chronic pain started in my spine shooting down my arm along with blurred vision and crushing pains in chest. My dr tested for everything including ultrasound of heart nothing conclusive a slight reading of past Ross river fever. I've since been to Neurologist had MRIs of spine and brain (no lesions) Lumber puncture (no abnormalities only side effects of screaming headaches for 5 days) VEP (ok) he says its not MS but can't explain the progressing symtoms and chronic pains spreading in my body.I have lost some of my arm senses and movement the other arm is following same way.It is hard to go from being very capable both mentally and physically (at 54 yrs old) to this in less than 6 months no one can tell me why? You and many of your contributors have the same journey of uncertainty thank you your stories have helped me keep my sanity.
ReplyDeleteMarc, I will probably be joining your "atypical" club.... I too have been somewhat a mystery for going on 4 years.... I am pretty darn sure I have MS, but so far the only medical professional that agrees it "could be" is my primary care and she is an NP...
ReplyDeleteIf I really think about it, I can go back to about age 20, my right knee would just act up from time to time, I always just figured it was because of being overweight/overstressed. I was in an abusive marriage at the time, I had a 5 year old kid, was working 5 jobs, and slowly I've just watched my body give up on me. I had to have a spinal fusion in 2003 (Johns Hopkins - Baltimore native here... but moved to Nashville in 2007). didn't really have any issues with the L5/S1 area other than some residual muscle spasms until last May. But 4 years ago my neck really started bothering me, an emrgency room trip and I have 3 herniated disc - NONE of which are herniated enough to explain my severe pain, my numbness, my inability use my hands, my weakness, etc. These things literally just sorta all started to pop up right around the same time. I began getting migraines that would make me debate cutting all my hair off just because my hair hurt that bad. continued... (i wrote too much to post in one comment).
me again...
ReplyDeleteNext Wednesday after 4 years of begging doctors I am FINALLY going to be seen by an MS doctor at Vanderbilt. I exhibit nearly all the symptoms of MS (list below) yet I've gone from walking with a bit of a limp to a cane to using a rollator, I don't have lyme, lupus, RA, or gobs of other autoimmune disorders, I am extremely vitamin D deficient and take RX 3x a weeks of 50,000 units and still can't get my levels up, (I did have Mono when I was in the 7th grade and understand that the virus that causes mono -- can't remember it's name now -- never actually leaves your system, i have a huge family history of MS - my great grandfather died of MS, a few of my cousins have MS all on maternal side -- I've seen 4 neurologists -- the first one sent me for an EEG and did a nerve conduction test -- I passed both -- didn't feel anything during the nerve conduction test of my arms as he stuck in needles and shocked me and even mentioned how shocked he was that I made it all the way through the test (and nearly fell asleep), but I couldn't feel anything... I get horrendous migraines, I have zero balance anymore and my two sons have had to pick me up off the floor more than once (try 6-8 times in the last 6 months) my eldest ended up moving back in with his wife and two children so I have a full time baby sitter during the day. I'm pretty convinced it's MS call it a gut feeling, I don't know, but I was normal just 4.5 years ago. It's driving me insane, all I want for Christmas is a diagnosis so I can move on to acceptance. maybe than social security can also make a decision on disability as well, i've been unable to work for 4 years, we are so close to losing our home and everything we have -- I've always overcome everything thrown at me, with grace and dignity, a teenage mom, from an abusive marriage, widowed at 23/24, my life could be a movie of the week on lifetime, you are so right about the why's... I just don't understand. I have an allergy to contrast so getting a clear MRI is difficult, I have 2 lesions on my spine, but because of my contrast allergy they are unsure if the lesions are hemangiomas or MS lesions... Typically I am really intelligent, I've owned my own business for more than 10 years, but this year in general I've not been able to keep on task at all, I am completely unfocused and my thoughts go everywhere, like that of an ADHD kid. I have no stamina anymore, or interest in things or friends either!
Common Problems
Fatigue -yes
Heat/Cold intolerance (heat) yes
Walking (Gait) Difficulties -yes
Numbness or Tingling -yes
Spasticity -yes
Weakness -yes
Vision Problems -yes
Dizziness and Vertigo -yes
Bladder Problems -yes
Sexual Problems (nothing medical, just no real hot n heavy desire, but I would never tell my husband no if asked)
Bowel Problems -yes
Pain -yes
Cognitive Changes -yes
Emotional Changes -yes
Depression/Anxiety -yes
Insomnia/Sleep Disruptions -yes
Less common symptoms
Speech Problems -yes (my sister and husband swear that I slurr speech at times, I don't notice or recognize it).
Swallowing Problems -yes
Tremor -yes
Seizures no
Breathing Problems no
Itching-yes - new symptom in the last few weeks I want to cut my finger tips off the only thing that help is me putting my hands in bags of ice!)
Headache -yes - migraines
Hearing Loss -yes
Secondary and tertiary symptoms
Frequent Bladder / urinary Tract infections -yes every time I go to the doctor (monthly) I have evidence of another infection.
really though, I just want a diagnosis so I can finally know and accept what it is that I am dealing with and get on with treatment or supporting care, whatever. just give what i have a name already, i don't know how much longer i can deal with this uncertainty.
thanks for listening. love your blog, I've been glued to it all night instead of doing what i'm supposed to be doing which is finishing this MS intake book.
So sorry to hear about all of your problems and difficulty getting a diagnosis. I can only imagine the frustration. Actually, I don't have to imagine the frustration, I've lived it.
DeleteThe MS team at Vanderbilt is very good, I understand, so hopefully they'll be able to give you something substantial to hang your hat on. I pretty much just excepted that whatever I have has no easy answers, so it really doesn't matter what they call it. Yes, it would be nice to have a firm diagnosis, but in the end, I don't think it would make much of a difference as far as treatment options go. Lots of times MS is given as a diagnosis when no other disease fits the bill. Doctors hate to say "I don't know", so they'll stick a name on it just to give it a label.
Given that you do have to lesions on your spine, which would be fairly typical for progressive MS, it certainly is possible that you do have Multiple Sclerosis. Have you ever had a spinal tap? Over 90% of MS patients have what are known as O-bands, which can help with a diagnosis.
Wishing you the best… Let me know how it goes, you can always email me at WheelchairKamikaze@Gmail.com.
Hi there - my name is Catherine and my fiancé was told he had ADEM 4 years ago. This was good news, as it ruled out MS. His right leg goes numb tho and it's getting worse. It used to only happen when he would really exert himself - and now it's all the time - - bad limp to the point of not being able to stand. But no pain. He has gone back to get tested for MS so many times over the years - MRIs all the time and lesions going away. Why is he getting worse? Hopefully his visit to the vascular surgeon will help tomorrow at Stanford ..
ReplyDelete