 Image via Wikipedia
Image via Wikipedia
A few months ago, I published a post about a radical new theory regarding Multiple Sclerosis, called the "Cerebrospinal Venous Insufficiency" theory, or CCSVI for short. I thought that now might be a good time to provide an update.
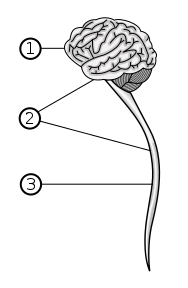
Just to review, several years ago researchers in Italy started looking at the vascular systems of MS patients, specifically by imaging the veins that are directly related to the central nervous system (the jugular and azygous veins). Incredibly, they found that in nearly all of the patients they studied there were blockages or abnormal narrowing of these very important vascular pathways. The researchers theorized that the vascular blockages they were finding could cause a reflux of blood back into the central nervous system, which in turn could lead to inflammation and edema, and eventually to a breakdown in the blood brain barrier, and thus be responsible for the damage seen in Multiple Sclerosis. About two years ago, the doctor leading this research, Dr. Paolo Zamboni, started performing modified balloon angioplasties on these areas of abnormality.
An interventional radiologist at Stanford University, Dr. Michael Dake, became interested in this research after it was brought to his attention by the activist wife of an MS patient. Dr. Dake traveled to Europe to meet Dr. Zamboni, and upon his return started doing some investigations of his own. He too found serious vascular abnormalities in nearly all of the MS patients he imaged. Based on these imaging studies, approximately 4 months ago Dr. Dake started performing endovascular surgery on these patients, placing stents in blocked veins to open up the areas of abnormality that he found.
To date, Dr. Dake has performed surgery on about 35 patients, most of whom have reported positive results as a result of the surgery. Although most of the patients who have undergone the procedure were not severely disabled due to MS, they all suffered from the usual array of MS symptoms, including cognitive dysfunction, heat intolerance, and severe fatigue. Many also suffered from varying degrees of motor and sensory dysfunction. Almost all have reported marked improvements in these areas.
Tragically, one of the patients who underwent the procedure died of a massive cerebral hemorrhage soon after, but the consensus is that the patient’s stroke was not directly related to the endovascular surgery that was performed. The blood thinning medication that was given postsurgery did contribute to the severity of this terrible event, but was not deemed to be a causative factor.
Dr. Zamboni recently published a summary outlining the results he's seen on the patients who were treated with his endovascular procedure, which he calls the "Liberation Procedure". In the 51 RRMS patients treated with the procedure, Dr. Zamboni claims a fourfold decrease in relapses. Furthermore, Dr. Zamboni performed the procedure on 18 patients who were suffering from acute relapses, and after surgery these patients recovered from their relapses in time periods ranging from four hours to four days. Dr. Zamboni cites this as "the best evidence that venous obstructions play a causative role in the complex pathogenesis of Multiple Sclerosis".
Dr. Zamboni and his team have organized a conference on "Venous Function and Multiple Sclerosis", to be held in Bologna, Italy on September 8 of this year. Several prominent US neurologists specializing in MS are expected to participate.
It's important to note that Dr. Zamboni's surgical results have been self-reported, and not subject to peer review. Additionally, no MRI imaging studies were done on his patients after they underwent the "Liberation Procedure", which would have been very valuable in assessing the impact the procedure had on the central nervous system lesions of those who underwent it.
Dr. Dake is planning on starting his own clinical study in September, 2009, which is expected to be limited to RRMS patients.
All of this information is extremely fascinating, and may offer a brand-new approach to understanding and treating Multiple Sclerosis. It's very important to keep in mind, though, that nothing has yet been proven, and that all of the results so far reported, as positive as they've been, have only come from two sources (Dr. Zamboni, and Dr. Marian Simka, who has done research on CCSVI in Poland). Scientific discipline requires that these results be replicated by independent researchers before anything definitive can be stated about this theory, and I expect that several groups will be attempting to do just that in the near future.
I personally find this research to be quite exciting, although I am maintaining a healthy skepticism regarding it. In my 6+ years as an MS patient, I've seen many such "theories du jour" generate tremendous enthusiasm, only to be disproven by the greater scientific community. In this case, though, my gut tells me that there might be something to this. I'm quite sure that this theory can't explain all cases of MS, but it does seem compelling enough to suggest that, at the very least, there is a subset of patients for whom the root cause of MS may not be neurologic or autoimmune, but vascular.
Research into the causes and treatments of Multiple Sclerosis has fallen almost exclusively into the realm of the neurology and neuroimmunology communities for the last 30 or so years. Though some impressive advances have been made, the disease has proven to be quite confounding when looked at from these perspectives. CCSVI offers a fresh approach at understanding the disease, and furthermore, offers the hope of some straightforward methods of treating it.
This research may turn out to be nothing but a flash in the pan, but there is the chance that it could revolutionize our understanding of Multiple Sclerosis. For this reason, I recommend that all MS patients pay close attention as the CCSVI story unfolds...
Update 11/21/09: Canadian television has done in a news report on CCSVI. Click here for the link.
Update 11/30/09: CCSVI: Separating Fact from Fiction. Click here.
An important post. The "blood thinners" needed to be taken when any foreign material is in contact with the blood such as the stents can be managed intelligently and maximising control of correct dosing. While the pathology lab will manage the dose protocol it is advisable to purchase a home testing unit now below a thousand dollars. The test strips are not cheap but worth it so time to time self testing can be carried out for any reason. I found this valuable as I have a prosthetic heart valve. The lab made mistakes, once phoned through someone else's dose, other times under dosed me big time exposing to risk of clotting the RNI level was the same as if I never took warfarin! The meter is useful when travelling or too far from a lab. The test strips storage improved, no need to keep them in the fridge. As to the new discovery one obstacle to overcome would be professional/institutional arrogance and ignorance of some experts. Open mind is needed and cooperation between the disciplines around the patients interest. Good nutrition, adequate exercise, close attention to antioxidants and anti-inflammatory natural and supplements, to control sub clinical inflammation implicated in many conditions. Dietary changes can and do alter INR the number denoting the level of blood clotting. So the home meter is helpful to track changes and keeping a record of food and drink intake can establish the picture we can take into account so we need to test not too often.
ReplyDeleteAt present many G.P.-s cardiologists and others are ignorant about inflammation. A few doctors are even hostile! Advocating and/or just interpreting for patients I was surprised what I witnessed! We need to be intelligent about alternative treatments and supplements. They are certainly valuable. The cooperation of both camp of doctoring is the best. Both camp has their charlatans and their heroes. WE often have to help the practitioners to help us to the highest degree. I hired my G.P. some 7 years ago after observing him. Some of my friends can't handle this and call me arrogant. Many years ago dropping in to see the doctor I was told he is not in today but there is someone else if I wanted to see. I told the receptionist O.K. I check him out. The unbelief of murmur swept the waiting room: "did you hear what he said?! HE IS GOING TH CHECK OUT THE DOCTOR!!!"-
Be well! joseph
Intriguing stuff.
ReplyDeleteI have often wondered why doctors seem reluctant to admit that many MSers also have migraine headaches (a VASCULAR condition).
But MSers almost universally complain about migraines.
This is incredibly interesting to me as I have a venous abnormality in my brain that I am told is genetic and I had a pulmonary embolism last year that they said is not related to MS yet can't find any other reason for. I am currently on blood thinners due to the blood clot. Very intriguing- will continue to follow this research. Please continue to keep us posted here!
ReplyDeleteIt does explain the problem of not being able to find a vein and the cold feet. now if we could just fix the damage done.
ReplyDeleteIs this a treatment that we can request or do we need to apply to be on a clinical trial?
ReplyDeletethere is a large, clinical trial now underway in Buffalo. My neurologist is part of the group involved in the trial. 16 years since dianosis for me. avonex and steroids have kept me functional and working, but vision, bladder, spasms and fatigue making things more difficult.
ReplyDeletethe thoery explains a lot, esp. the presence of iron deposits seen on brain mri from red blood cells.
Let's just say I have had this MonSter since 1980, when I was 16. I’m Dxed with MS, I get a sucker and a free tee-shirt and the doctor says “It's tough but we can’t do anything. See you again in twenty year for a checkup and maybe a rx for a wheel chair”. Let’s think big picture, fast forward to 2010. Sharp primary care doctor noticed a twitch in my eyes when taking a physical for high school sports. She sends me to an optometrist that sends me to a neurologist that sends me for trancranial Doppler sonogram. The findings show reflux or stenosis in the veins leading from the brain. I undergo successful angioplasty and optimal blood flow is restored. End of story.
ReplyDeletehello, thanks for posting articles like these.This is something very interesting and relevant to the subject.Keep posting articles like these.
ReplyDeleteI understand that the neurologist team at Stanford forced Dr Dake to terminate his research. Could it be because he is not one of "them".
ReplyDeleteAlso the University of Buffalo trials are operating on one patient a week-- maybe more since July 1. That would be about 50 patients. Any early results??
I get a sucker and a free tee-shirt and the doctor says , I will take care .
ReplyDeleteYou made some good points .I did a little research on the topic and found that most people agree with your blog. Thanks.
ReplyDeleteYour article is really Very significant for us ,because i am student and also searching for that type of articles and I think the representation of this article is actually superb one. This is my first visit to your site.
ReplyDelete