It's now been over 18 months since the news of Dr. Zamboni's vascular theory of MS, the CCSVI hypothesis, first made its way into the consciousness of the greater Multiple Sclerosis patient population. Touched off by news reports on Canadian television channel CTV, an inferno of hope raced through MS patients worldwide, and a firestorm of controversy regarding almost every aspect of the hypothesis was ignited, a conflagration that seems to only burn more intensely with each passing week. The relatively simple CCSVI hypothesis (which postulates that blockages in the veins draining the central nervous system lead to or contribute to the MS disease process) has managed to pit physician against physician, physician against patient, and patient against patient. While the various factions duke it out, an estimated 15,000-20,000 MS sufferers have undergone CCSVI venoplasty, with a wide variety of resulting outcomes, ranging from dramatic benefit to no benefit whatsoever to, in rare cases, a worsening of disease symptoms.
Several key questions have emerged regarding CCSVI during the last year and a half, primary among them whether or not CCSVI and MS have any link whatsoever, and if so, whether the venous anomalies collectively known as CCSVI are the cause or an effect of the disease. We've seen a steadily increasing flow of CCSVI research results, providing enough conflicting data to fuel all sides of the argument. As with all things Multiple Sclerosis, CCSVI presents a complex picture, and despite evangelical believers/nonbelievers on all sides of the squabble, at present the ultimate outcome of the CCSVI conundrum is as clear as mud. Here then is a brief look at some of the issues currently being batted about, with some small attempt on my part to make some sense of it all.
My personal belief is that CCSVI and MS do indeed have a relationship, at least in some MS patients. However, I acknowledge that my opinion is based primarily on anecdotal evidence, and anecdotal evidence alone is not enough to state anything with scientific certainty. Despite the insistence of many in the CCSVI advocacy community, the link between CCSVI and MS has not yet been established with evidence that measures up to the scientific standard. On its face, the basic premise of CCSVI, that restricted blood flow through the central nervous system, caused by vascular abnormalities that are very likely congenital, slowly cause damage to the CNS over the course of decades, eventually becoming significant enough to result in a clinical diagnosis of Multiple Sclerosis, seems simple and makes perfect sense. Yet upon closer inspection, the picture is not quite so clear-cut.
There have been several very convincing studies demonstrating that venous abnormalities now known as CCSVI occur more often in MS patients, and even in patients with other neurologic diseases, than in healthy control subjects. Conversely, there have also been quite a few studies disputing this. Almost all of these studies, pro and con, have relied on noninvasive imaging techniques (Doppler ultrasound or MRV) to ascertain the presence of these abnormalities. Unfortunately, neither of these noninvasive imaging techniques has proven to be entirely accurate, though Doppler ultrasound, in the hands of a skilled and well trained technician, does appear to be the more reliable of the two techniques. Still, we have research groups reporting widely divergent findings, and some of that divergence could possibly be attributed to the relative inaccuracy of the diagnostic methods being utilized.
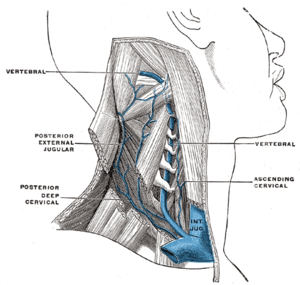
Complicating matters further is the fact that human venous anatomy, with a few exceptions, has been very little studied. So little, in fact, that no clear-cut definition of "normal" exists when it comes to the anatomy of the veins that drain the central nervous system. It had previously been assumed that since the veins in question had so many built-in redundancies, any blockages encountered would be easily compensated for. While the Interventional Radiologists performing the CCSVI treatment procedure are reporting that the overwhelming majority of MS patients are indeed displaying a large number of venous abnormalities, we cannot state with any certainty that a significant portion of the healthy population does not also present with such abnormalities.
What are desperately needed are trials using catheter venography to ascertain the prevalence of CNS venous abnormalities in healthy control subjects. However, there are some ethical questions involved in performing this minimally invasive procedure simply for research purposes. Although the risk is low, catheter venography, like any invasive procedure, does carry with it the potential for dangerous complications, and the prospect of exposing healthy subjects to these risks has inhibited such studies from taking place. Until it can be established beyond dispute that vascular abnormalities in the jugulars, azygos, and other veins that drain the CNS are more prevalent in MS patients than in the general population, the question of the CCSVI/MS relationship will not be put to bed.
Let's assume, though, based on the anecdotal reports, that there is a connection between CCSVI and MS. The big question then becomes whether CCSVI is the cause of the disease, or an effect of the Multiple Sclerosis disease process. Again, there is enough conflicting data to support both sides of the argument.
Those who support CCSVI as the cause of MS site several compelling reasons for their belief. One of these is that many of the abnormalities being seen in the veins of MS patients, such as anomalous membranes and fused valves, appear to be congenital in nature, that is, patients have had them since birth (click here). If these defects are congenital, and occur in greater preponderance in MS patients than the healthy population, it would seem reasonable to assume that they play a causative role in MS disease etiology. Another argument in favor of CCSVI as the cause of MS is the growing body of evidence that suggests that nervous system tissues in MS patients are damaged before the immune system comes into play (click here for one such study), findings that would seem to contradict the prevailing theory of MS, the "autoimmune theory". The autoimmune theory states that, for reasons unknown, the immune systems of MS patients go rogue and start attacking the patients' own central nervous system tissues. If some studies done within the last decade are correct, and CNS damage occurs before immune system involvement, this would apparently discredit many of the basic assumptions of the autoimmune theory, and CCSVI provides an explanation as to how this damage occurs.
While I've long held the autoimmune theory in contempt, and I'm convinced that the aberrant immune response seen in MS patients is a symptom of some larger underlying and as yet undiscovered cause, I'm not sure that cause is CCSVI. While the CCSVI hypothesis does in some ways elegantly account for some of the mysteries surrounding MS (the venocentric nature of MS lesions, the reduced volume of blood flow through MS brains, etc.), it does not account for several of the more confounding aspects of the disease. It's difficult for CCSVI to explain the geographical distribution of the MS population, which sees a far greater prevalence of MS the further away one gets from the equator (click here). Related to this geographic distribution, CCSVI also can't explain some of the migratory observations made in regard to disease prevalence (click here). When a person below the age of 15 migrates from an area of higher disease prevalence to one of lower prevalence, they take on the characteristics of their new home. When the migrant is over the age of 15, though, they retain the propensity for the disease of the area they migrated from. In other words, a person under the age of 15 migrating from Maine (high prevalence) to Florida (low prevalence) has the same low chance of getting the disease as a Florida native. However, older migrants retain the higher chance of getting the disease seen in Maine. Furthermore, children of these older migrants, born after the move south, take on the same lower chance of developing MS as children born to the native population.
Similarly, CCSVI cannot account for the existence of "MS clusters", which are small concentrations of population in which MS appears to be epidemic (click here). The most famous of these clusters is in the Faroe Islands, an island group situated between the Norwegian Sea and the North Atlantic Ocean. Prior to World War II, MS was virtually unknown among the native islanders. During World War II, the British, who have a high incidence of MS, occupied the island, and subsequent to this occupation, MS has become epidemic among the native population. Another such cluster was recently identified in a small town in Ohio, where over two dozen MS cases were discovered within a six block radius.
The geographic and migratory components of MS epidemeology, as well as the existence of MS clusters, are heavily suggestive of an environmental (infectious or toxic) element to the MS disease process, and indeed, recent studies have linked several viruses, most of them in the herpes family, to MS. Just within the last week or two, a study out of Taiwan, which looked at hundreds of thousands of subjects, found that people suffering an outbreak of shingles, a painful skin condition caused by the varicella zoster virus (which also causes chickenpox), are three times as likely to develop MS within the year as those who didn't suffer from shingles (click here). Likewise, the Epstein-Barr virus has also been cited as a possible infectious trigger of the disease, with some scientists stating that if a patient isn't infected with EBV, they won't get MS (click here).
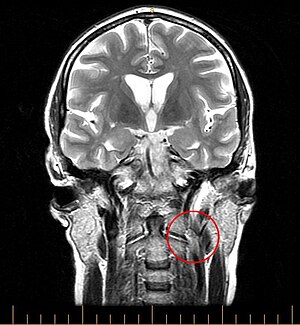
Another potential problem with CCSVI as the cause of MS is the inflammatory patterns seen in patients afflicted with the disease. According to CCSVI theory, disrupted blood flow through the CNS creates damage and inflammation to the cells contained within, through a variety of possible mechanisms. This would lead one to expect that the longer the condition persisted, a patient's levels of inflammation would slowly increase over time, in a steady upward slope. However, in reality, RRMS patients see their greatest amount of inflammation early in the disease, during its relapsing remitting stage. Once the disease moves into the progressive stage, and RRMS turns into SPMS (normally within 10-15 years when left untreated) inflammation levels decrease dramatically. Patients with PPMS, who start out with progressive disease, very often show very little signs of CNS inflammation. As a matter of fact, this lack of inflammation, seen as enhancing lesions on MRI images, is a hallmark of progressive disease. This is why anti-inflammatory therapies such as steroids generally have little effect on patients with progressive illness.
Of course, none of this directly contradicts the idea that CCSVI may play some causative role in the disease of some MS patients, but it strongly argues against the idea that CCSVI is the primary cause of the disease.
Some compelling evidence that CCSVI may be an effect of MS has been presented by several researchers, most notably Dr. Robert Zivadinov and the researchers at the Buffalo Neuroimaging Analysis Center. Although Dr. Zivadinov's findings have been savaged by some of the most fervent "CCSVI as cause" proponents, the totality of the research done under his direction does point to the possibility that at least some of the venous abnormalities now called CCSVI are a result of the MS disease process. Although Dr. Zivadinov's opinions only recently made headlines (click here), he in fact implied them in research presented in October, 2010 at the annual ECTRIMS (European Committee on Treatment and Research in Multiple Sclerosis) conference. One paper presented at that time demonstrated that the severity of CCSVI increases with the severity of Multiple Sclerosis symptoms experienced by patients, and with a more advanced disease course (click here). These findings were backed up by papers presented by researchers from Beirut (click here) and Italy (click here). Another study presented by Dr. Zivadinov found that subjects who presented with CCSVI had significantly more lesions and brain atrophy as measured by MRI than those MS patients without vascular abnormalities (click here). Yet another investigation presented by Dr. Zivadinov looked at the correlation between a gene implicated with MS, and CCSVI, and found that the data supported an association between MS disease progression and CCSVI separate from the suspect gene. The implications of these findings are that CCSVI could be a risk factor in developing the disease, or a result of the progression of MS (click here).
Additionally, it would seem to me that the high rate of restenosis in patients who have undergone CCSVI treatment venoplasty could also hint that CCSVI is more an effect rather than the cause of MS. Despite the wide range of treatment methodologies being employed, patients are still experiencing a re-narrowing of their previously unblocked veins far too frequently. This has been seen even in patients who have had stents placed in their veins, only to see their veins stenosing in areas not stented. If CCSVI were an effect of the MS disease process, one would expect to see repeated restenosis of the veins as that disease process continued to impact a patient's vasculature.
So then, what conclusion can be drawn? Is CCSVI the cause of MS, an effect of the disease, or does it have no relation to Multiple Sclerosis at all? My honest belief is that the answer could be all three, depending on the individual patient.
Multiple Sclerosis is a remarkably heterogeneous disease, meaning that it impacts different patients in vastly different ways. Across the wide spectrum of MS patients, the primary symptom of the disease may be fatigue, cognitive dysfunction, muscle weakness, spasticity, eye trouble, nerve pain, or any combination thereof. Some patients can have the disease for decades and show very little physical disability, while others find themselves in a wheelchair (or worse) in less than 10 years (sometimes much less). Some patients have a great many lesions and very little disability, others have few lesions but devastating disability. Confounding the issue even more, MS comes in several different flavors, from Relapsing Remitting to Primary Progressive, and evidence suggests that the disease process at work in progressive disease may be quite different than that underlying Relapsing Remitting MS.
Given such a wide array of disease presentations, and thus the likelihood that a variety of mechanisms may be at play, it could very well turn out that CCSVI plays no role at all in the disease of some patients, a more causative role in the disease of others, and could be an effect of MS in yet another patient population. Very likely the line between cause and effect may be quite blurred, with CCSVI playing an exacerbating role in a disease that almost certainly has, in addition to a vascular component, very strong genetic and infectious components as well. The mix may be dramatically different from patient to patient, and indeed, CCSVI may be THE major factor in the disease of some patients, but play absolutely no role in the disease of others.
This may be reflected in the breakdown of outcomes reported by some of the Interventional Radiologists doing the CCSVI treatment procedure. The most widely quoted is Dr. Gary Siskin, of Albany New York, whose group has done over 700 procedures. Dr. Siskin has found that one third of his patients experience dramatic improvements, another one third experience mild improvements, and a final one third experience no improvement whatsoever. Further complicating this equation is the definition of just what constitutes a dramatic improvement. For somebody who's most disabling symptom is fatigue, a lifting of that fatigue would undoubtedly be called dramatic. For somebody more disabled, like I am, a lifting of fatigue, while certainly welcome, would hardly be defined as a dramatic improvement.
As I stated earlier, clear as mud…